Case Report - (2023) Volume 8, Issue 1
Atypical Meningioma with Chronic Subdural Hematoma: A Case Report
Maria Cecilia Ong-Lingan*
Department of Neurological Surgery, University of Santo Tomas Hospital, Philippines
*Correspondence:
Maria Cecilia Ong-Lingan,
Department of Neurological Surgery, University of Santo Tomas Hospital,
Philippines,
Email:
Received: 02-Jan-2023, Manuscript No. IPJNO-22-15480;
Editor assigned: 04-Jan-2023, Pre QC No. IPJNO-22-15480 (PQ);
Reviewed: 18-Jan-2023, QC No. IPJNO-22-15480;
Revised: 23-Jan-2023, Manuscript No. IPJNO-22-15480 (R);
Published:
30-Jan-2023, DOI: 10.21767/2572-0376.23.8.001
Abstract
We report a case of a 42 year old Filipino female teacher right handed with atypical meningioma and concomitant
chronic subdural hematoma who presented with persistent headache associated with nausea, vomiting and
sensitivity to light and loud noise. With a positive family history of migraine, no previous history of trauma, and
unremarkable past medical history, patient was initially treated as a case of migraine type headache and was given
Topiramate, Hydroxyzine, Flunnarizine and Metoclopramide, which did not provide relief of symptoms. Cranial
MRI with gadolinium contrast showed a right parietal convexity extra axial mass with concomittant right frontotemporoparietal
chronic subdural hematoma. Histopathologic examination revealed Atypical Meningioma WHO
Grade II, positive for vimentin and EMA immunohistochemical staining. The mainstay treatment still for Atypical
Meningioma with chronic subdural hematoma is evacuation of the hematoma followed by gross total resection
of the said extra axial mass and adjuvant radiation therapy. Benign tumors such as meningioma rarely present
with tumor related hemorrhages, but as seen from this case, subdural hematoma formation whether acute or
chronic is a possibility.
Keywords
Meningioma; Subdural hematoma; Intracranial hemorrhage; Headache
INTRODUCTION
Meningioma, a well encapsulated, benign tumor, is the second
most common primary intracranial mass lesion accounting to
33.8% of all cases [1,2]. It has a female preponderance with
increasing incidence with age. According to a population based
study from Germany, the 10 year overall survival rate ranges
from 72%-91% with cumulative incidence recurrence of 9% [3].
Majority of them present with headache, followed by seizures,
ranging from 25%-40% [3-5]. Despite its innately high vascularity,
they rarely present with intracranial hemorrhage, unlike
other tumors such as metastases and high-grade gliomas [6].
The reported incidence of hemorrhagic meningioma is 0.5%-
2.4% [7,8]. This scenario is more commonly seen in post-embolization
or as part of complication of radiotherapy, namely,
radiation necrosis. The subarachnoid space is the most common
site of hemorrhage, followed by the intracerebral and intratumoral
regions [9,10]. On the other hand, the occurrence
of spontaneous subdural hematoma whether acute or chronic
type is very rare.
The occurrence of bleeding from a meningioma is said to be
an interplay of several pathogenetic mechanisms such as the
following:
• Enlarging mass impinging on dural sinuses leading to venous
hypertension
• Rupture of distended, fragile, thinned walled abnormal tumoral vessels brought about by tumoral growth [1,9].
• Stretching of subdural bridging veins secondary to tumoral
expansion [1,6,11].
• Direct tumoral invasion with concomitant expression of
vascular endothelial growth factor by tumor cells especially
the malignant types [1,6,9-11].
• Formation of capsule like dura similar to the outer
neomembrane of chronic subdural hematoma invaded by
meningioma cells exuding hematoma expansion into the
subdural space [11].
• Release of vaso-active and fibrinolytic substances from
mast cells causing neovascularization and necrosis, respectively,
with subsequent blood vessel wall rupture [1,6,11- 13].
Based on the data available from the period of 2011 to 2020
from the section of Neurological Surgery at the University of
Santo Tomas Hospital, only 0.05% (1 out of 208) of patients with
definitive diagnosis of meningioma had associated non-traumatic
subdural hematoma, signifying the rarity of such case. At
present, only 20 reported cases of chronic subdural hematoma
associated with meningioma have been reported in the literature
studies [9] (Table 1).
| No. |
Author |
Year |
Sex |
Age |
CSDH |
Meningioma |
| Side |
Side |
Location |
Histology |
Outcome |
| 1 |
Cusick and Bailey |
1972 |
F |
47 |
Bilateral |
Right |
Convexity |
Transitional |
Dead |
| 2 |
Modesti, et al. |
1976 |
F |
49 |
Left |
Left |
Parasagittal |
Meningothelial |
SD |
|
|
|
M |
69 |
Left |
Left |
Convexity |
Meningothelial |
GR |
| 3 |
Walsh, et al. |
1977 |
F |
77 |
Right |
Right |
Olfactory groove |
Meningothelial |
Dead |
| 4 |
Sakai, et al. |
1981 |
M |
36 |
Right |
Right |
Sphenoid ridge |
Meningothelial |
Dead |
| 5 |
Baskinis, et al. |
1984 |
M |
68 |
Right |
Right |
Convexity |
Angiomatous |
GR |
| 6 |
Tomita, et al. |
1985 |
F |
61 |
Right |
Right |
Convexity |
Meningothelial |
GR |
| 7 |
Wang, et al. |
1985 |
F |
62 |
Left |
Left |
Convexity |
n/a |
n/a |
| 8 |
Itoyama, et al. |
1987 |
F |
63 |
Bilateral |
Left |
Sphenoid ridge |
Transitional |
GR |
| 9 |
Chen, et al. |
1992 |
M |
19 |
Left |
Left |
Convexity |
Meningothelial |
MD |
| 10 |
Pozzi, et al. |
1993 |
F |
73 |
Left |
Left |
Convexity |
Transitional |
n/a |
|
|
|
F |
85 |
Left |
Left |
Convexity |
n/a |
n/a |
| 11 |
Popovic, et al. |
1994 |
F |
47 |
Right |
Right |
Convexity |
Meningothelial |
n/a |
| 12 |
Tanaka, et al. |
1994 |
F |
47 |
Right |
Right |
Convexity |
Meningothelial |
GR |
| 13 |
Sinha and Dharker |
2001 |
M |
68 |
Left |
Right |
Convexity |
n/a |
GR |
|
|
|
F |
70 |
Left |
Right |
Convexity |
n/a |
GR |
| 14 |
Di Rocco, et al. |
2006 |
M |
72 |
Right |
Right |
Convexity |
Meningothelial |
GR |
|
|
|
M |
74 |
Left |
Left |
Convexity |
Transitional |
GR |
| 15 |
Czyz, et al. |
2011 |
F |
69 |
Bilateral |
Bilateral |
Parasagittal |
n/a |
GR |
| 16 |
Nery, et al. |
2017 |
F |
85 |
Left |
Left |
Convexity |
Microcystic |
GR |
|
|
Present report |
F |
42 |
Right |
Right |
Convexity |
Atypical |
GR |
Abbreviations: (CSDH) Chronic Subdural Hematoma; (GR) Good Recovery; (MD) Moderate Disability; (n/a) Not Applicable; (SD) Severe Disability
Table 1: Summary of previously reported cases of meningioma associated with chronic subdural hematoma.
Case Presentation
Patient Information
The patient is a 42 year old, non-hypertensive, non-diabetic, female,
teacher from Manila, Philippines who presented with a 2
years history of intermittent, unilateral, non-throbbing, non-radiating
headache relieved by rest. Until 5 days prior to admission,
there was increasing frequency and severity of the headache
now accompanied by nausea, vomiting, sensitivity to light
and loud noise; no associated weakness, seizures nor loss of
consciousness noted; she self-medicated with paracetamol and mefenamic acid, which did not afford relief of symptoms. On
the 3rd day of symptoms, she sought consult at a local hospital in
the Philippines, managed as a case of migraine-type headache,
given Topiramate, Hydroxyzine, Flunnarizine and metoclopromide
affording no relief of symptoms. On the 5th day, the family
decided to bring her to another local hospital, where she was
subsequently admitted and referred to neurosurgery with the
primary consideration of a convexity meningioma coexistent
with subdural hematomas of varying ages at the right frontotemporoparietal
convexity as seen on the imaging result.
Clinical Findings
On admission, neurological examination revealed intact mental
status and cranial nerve functions. Mini-mental status examination
and MOCA-P showed normal results with a score of 28/30
and 30/30 respectively. On gross examination, there were no
fasciculations, atrophy or hypertrophy of the muscles on all
limbs. Motor examination showed no weakness on all extremities
(5//5 motor strength, Medical Research Council). She was
normo-reflexive (+2) on bilateral biceps, triceps, brachioradialis,
knee and ankle jerk. No frontal release signs (such as palmomental
sign, glabellar tap, rooting reflex, sucking reflex) nor parietal signs (such as apraxia, astereognosia, Right/left confusion,
finger agnosia) were appreciated. Cerebellar examination was
normal. No sensory deficits were elicited. Neither observable
long tract signs nor meningeal signs were noted. Eastern Cooperative
Oncology Group (ECOG) score and Karnofsky Performance
Status score were 1 and 80%, respectively on admission
and improved to 0 and 100% respectively upon discharge.
Diagnostic Assessment
Basic laboratory examinations including CBC, Sodium, Potassium,
creatinine, coagulations studies (PT, aPTT), urinalysis, 12L
ECG and Chest x-ray were done and all revealed unremarkable
results. Having been unsuccessfully treated as a case of migraine
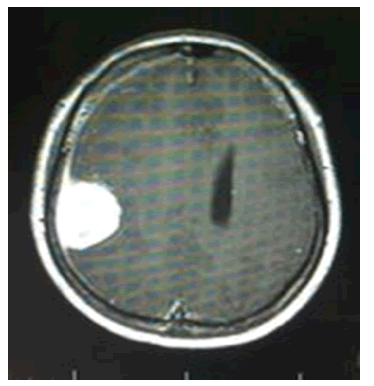
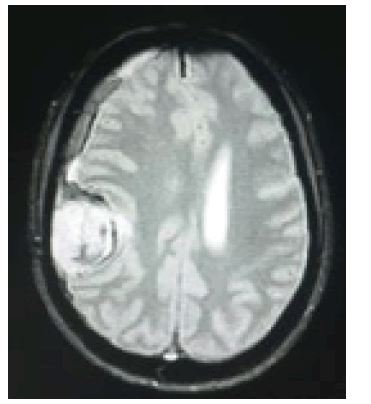
type headache, a cranial MRI with gadolinium contrast
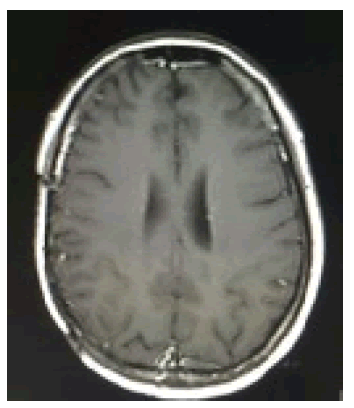
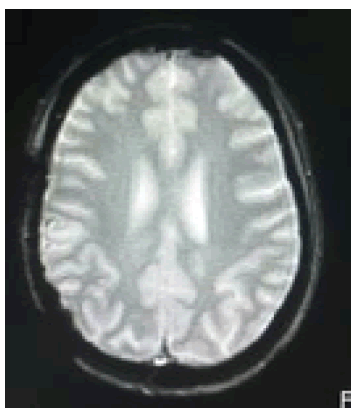
done revealed a 4.1 × 2.8 × 3.8 cm heterogeneously enhancing
right parietal extra axial mass along with crescentic subdural
lesion at the right frontotemporoparietal area, measuring approximately
0.9 cm in widest diameter with a midline shift of
1.2 cm, associated with focal areas of necrosis, as well as intralesional
blooming dark signals that likely represented blood
products exhibiting mass effect and surrounding perilesional
vasogenic edema (Figures 1 and 2).
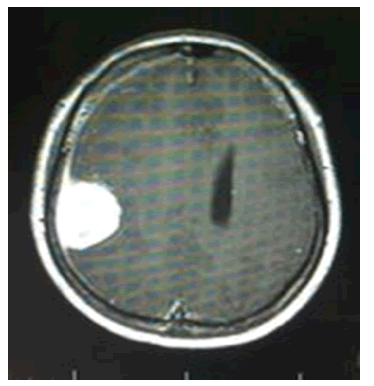
Figure 1: (T1+C) Large, avidly enhancing extraaxial mass ms. 4.1 x 2.8 x 3.8 cm at the right parietal region. (Pre-operative MRI).
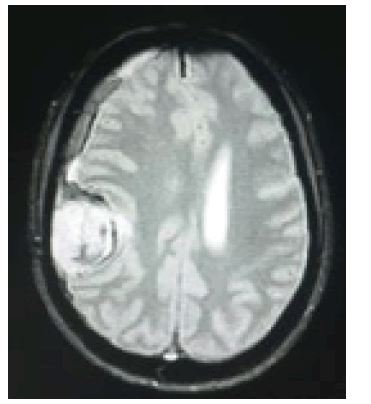
Figure 2: (GRE) crescentic extraaxial blooming dark subdural fluid collection signal at right frontotempo-parietal (Pre-operative MRI).
Intervention
Preoperatively, she was started on Mannitol 100 cc/IV q6 and
Dexamethasone 5 mg/IV q6 to facilitate brain relaxation during
the procedure. Prophylactic anticonvulsant, Levetiracetam 500
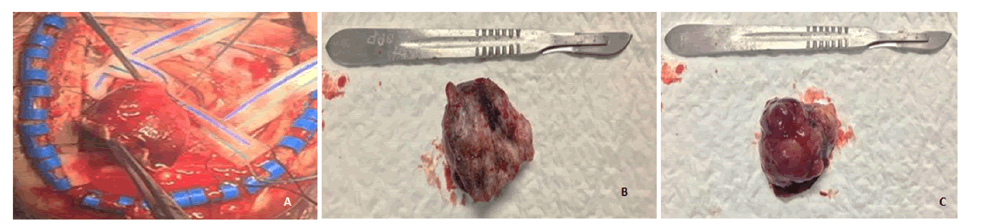
mg/tab 1tab q12, was likewise given. Operation done was right
parietotemporal craniotomy for Simpson’s Type I excision of
right parietal convexity meningioma and evacuation of subdural
hematoma. Intraoperatively, approximately 4x3x2.7 cm soft
to rubbery, multilobulated light to dark brown mass with dural
measuring 4x3.8x0.1 cm was excised and evacuated roughly 30
cc of non-clotted blood. No vascular lesions such as aneurysms,
arterio venous malformations or dural arterio venous fistulas
seen during the procedure (Figure 3).
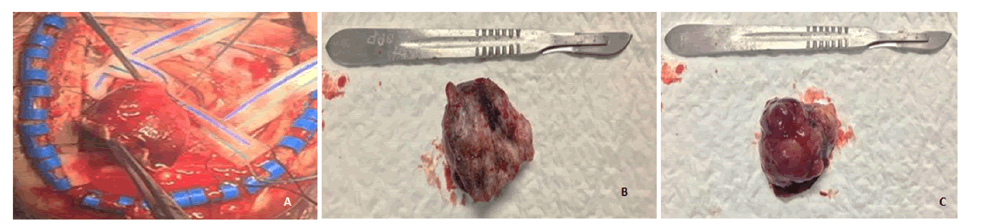
Figure 3: light brown-dark brown, multilobulated, soft to rubbery tissue ms. 4 x 3.3 x 2.7 cm and weighs 15 grams, with an attached dura ms. 4 x 3.8 x 0.1 cm.
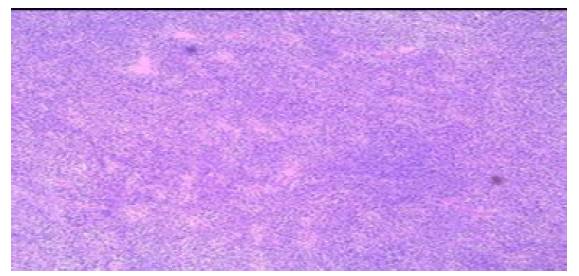
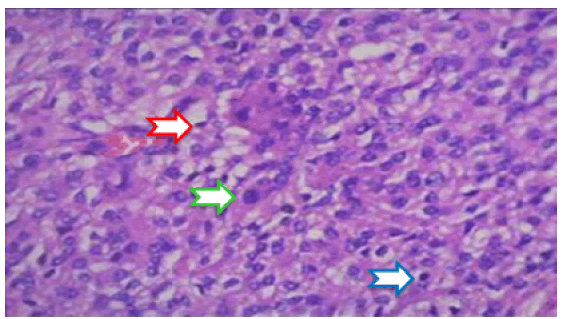
Histopathological examination revealed atypical cells with round
to ovoid nuclei and scanty cytoplasm admixed with spindle cells
of varying sizes, mitotic activity of 3-9 per 10 high power field,
in addition to a positive immunohistochemical staining for Epithelial
Membrane Antigen (EMA) and Vimentin; characteristics
consistent with Atypical Meningioma, WHO grade II (Figures
4 and 5). Eight weeks after gross total excision of tumor, she
subsequently received Intensity Modulated Radiation Therapy
(IMRT) with prescription dose of 180 cGy for 30 fractions with
Planning Target Volume (PTV) 54 Gy.
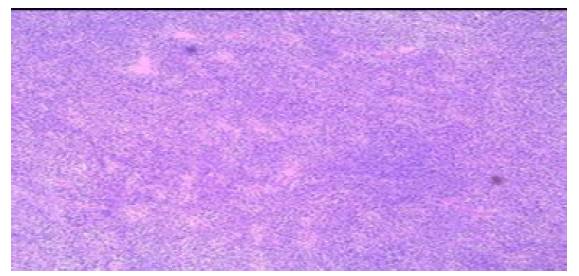
Figure 4: H and E Stain (low magnification).
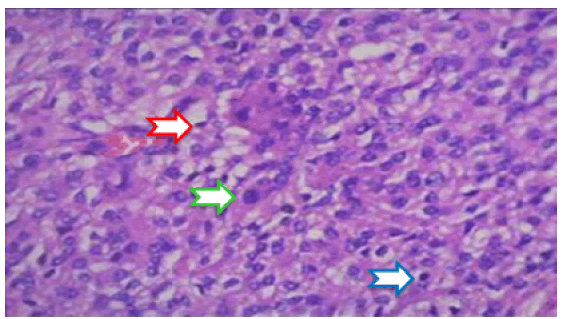
Figure 5: H and E Stain (high magnification). Atypical cells w/ round to ovoid nuclei (Green Arrow). Spindle Cells w/ scant cytoplasm (Yellow Arrow). Mitotic Activity of 3-9/high power field (Blue Arrow).
Result
Cranial MRI with contrast was done pre and post-adjuvant radiotherapy,
one month and seven months post-operation respectively.
Results showed absence of previously demonstrated
extra axial mass and chronic subdural blood at the right temporoparietal convexity with regression of the dural thickening
(Figures 6 and 7). Post radiation therapy, the patient developed
scalp dermatitis at the post-operative site, which was managed
medically.
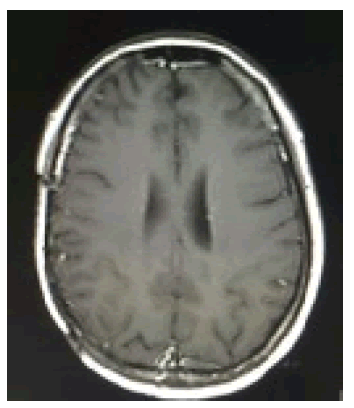
Figure 6: (T1+C) absence of previously noted right parietal mass (Post-operative MRI).
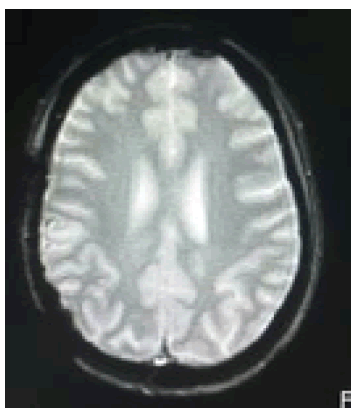
Figure 7: (GRE) absence of right subdural hematoma (Post-operative MRI).
Upon writing of this report, the patient is on Levetiracetam 500
mg/tabs 1 tab twice daily. A focal seizure episode was noted last
June 2020 likely due to a missed dose of anticonvulsant however,
no noted recurrences thereafter. She was advised repeat
cranial MRI with gadolinium contrast one year post tumor surgery
for surveillance.
Discussion
The key points of this present case are as follows:
• Not all hemorrhagic intracranial brain tumors are malignant.
• Based on the reported literature above, hemorrhagic meningioma
specifically of chronic subdural type is more commonly
seen in the elderly age group greater than 60 years
of age in 67% of cases, with a female predominance (2:1),
convexity area in location (76.1%), and is usually seen ipsilateral to the tumor (80.9%).
• The more common meningioma histology with concomitant
chronic subdural hematoma is seen in the benign type
namely, Meningothelial, Transitional, Angiomatous and Microcystic
(in decreasing order of frequency) rather than the
aggressive, atypical type.
• 57% (11 out of 21) of patients who have meningioma with
concurrent subdural hematoma had good functional outcome.
Patient Anonymity, Consent and Confidentiality
Written informed consent was obtained from the patient for
writing and possible publication of this case report and the accompanying
radiologic and histopathologic images. All personal
information regarding the patient has been kept strictly confidential
and patient identifiers such as name, location, date of birth, contact numbers, etc. have been removed from the manuscript
and the presented illustrations. Patient’s anonymity and
confidentiality is protected at all times by non-disclosure of any
personal information that will identify the individual when the
study is published or presented. A breach of confidentiality may
occur if the information is used in any other way. The patient
fully understood the content of the consent in English version.
A copy of the written consent form was provided to the patient
prior to the start of the study. She is aware that by participating
in this case report, she authorized the principal investigator to
have access to her personal medical records; the Research Ethics
Committee (REC) will have access as well, for the purpose of
verification prior to presentation of this case.
Ethical Considerations
This study is subjected to the University of Santo Tomas Hospital
Research Ethics Committee (REC) for approval prior to study
commencement, and will be modified according to the REC’s
requirements and modifications. The informed consent was obtained via zoom teleconference between the patient and me as
her attending physician together with her husband as witness.
During the conference, several key points were discussed with
the patient correspondent to the Philippine National Ethical
Guidelines 2017 with following ethical principles/guidelines:
Beneficence
This study may not directly benefit the patient reviewed in this
research but any information or conclusion that will be drawn
in this study shall greatly benefit future patients with the same
condition and/or possibly devise clinical practice guidelines that
will standardize management requiring the same medical and/
or surgical intervention. This would aid the future neurosurgeon
in their decision making, when presented with a patient
who complains of migraine type of headache unrelieved by intake
of analgesics.
Risks
The research study will not impose any risk to the subjects nor
will it violate their rights as study participants. The main risk for
the patient in this study would be a breach in confidentiality associated
with the chart review. The proper implementation for
confidentiality shall be discussed in the following paragraph. Although
the risk is always present, the numerous benefits clearly
outweigh the risk associated.
Privacy and Confidentiality of Information
The identity of patient in the study will be strictly safeguarded
in accordance with the Republic Act 10173 known as the Data
Privacy Act (2012). Data shall be obtained from reviewing patient’s
chart from the University of Santo Tomas records section.
Pictures shall be obtained from the Department of Radiology
and Pathology after obtaining informed consent from the
patient and approval of the hospital’s Data Privacy Officer. No
other personal information will be disclosed in the event that
the research study is published or presented.
These will then be stored safely in a locked cabinet located
within Department of Surgery Staffroom. All data transcribed via computer shall be password protected. Only the primary investigator will have access to data of any kind from this study.
Saving of electronic data to an external drive is restricted. Any
printed/written files shall be dispensed via paper shredder and
will be discarded to a secured bin once study has been completed.
Justice
No compensation, in monetary form or in kind, will be given to
any personalities involved in this study nor will the researcher
not receive any specific grants from any agency in the public,
commercial or not for profit sector.
Conclusion
This study showed that benign intracranial tumors can also
present with hemorrhage. Prompt investigation is warranted
for medically intractable headaches.
Conflict of Interest
There is no potential conflict of interest that could be perceived
as prejudicing the impartiality of this research work.
Acknowledgement
None.
References
- Aloraidi A, Abbas M, Fallatah B, Alkhaibary A, Ahmed ME, et al. (2019) Meningioma presenting with spontaneous subdural hematoma: A report of two cases and literature review. World Neuro surg. 127:150-154.
[Crossref] [Google Scholar] [PubMed]
- Wiemels J, Wrensch M, Claus EB (2010) Epidemiology and etiology of meningioma. J Neurooncol. 99:307-314.
[Crossref] [Google Scholar] [PubMed]
- Hollaczek B, Zampella D, Urbschat S, Sahm F, Deimiling AV, et al. (2019) Incidence mortality and outcome of meningiomas: A population-based study in germany. Cancer Epidemiol. 62:101562.
[Crossref] [Google Scholar] [PubMed]
- Chozick BS, Reinert SE, Greenblatt SH (1996) Incidence of seizures after surgery for supratentorial meningiomas: A modern analysis. J Neurosurg. 84:382.
[Crossref] [Google Scholar] [PubMed]
- Englot d, Magill ST, Han SJ, Chang EF, Berger MS, et al. (2016) Seizures in supratentorial meningioma: A systematic review and meta-analysis. J Nueorsurg. 124(6):1552-1561.
[Crossref] [Google Scholar] [PubMed]
- Kim JH, Gwak HA, Hong EK, Bang CW, Lee SH, et al. (2015) A case of benign meningioma presented with subdural hemorrhage. Brain Tumor Res Treat. 3(1): 30-33.
[Crossref] [Google Scholar] [PubMed]
- Lin RH, Shen CC (2016) Meningioma with purely intratumoral hemorrhage mimicked intracerebral hemorrhage: Case report and literature review. J Med Sci. 36:158-61.
[Crossref] [Google Scholar]
- Pressman E, Penn D, Patel NJ (2020) Intracranial hemorrhage from meningioma: 2 Novel risk factors. World Neurosurg. 217-221.
[Crossref] [Google Scholar] [PubMed]
- Rocco FD, Mannino S, Puca A, Lauriola L, Pompucci A (2006) Intracranial meningiomas associated with non-traumatic chronic subdural hematoma. Acta Neurochir. 148:1097-1102.
[Crossref] [Google Scholar] [PubMed]
- Matos D, Pereira R (2020) Meningioma-related subacute subdural hematoma: A case report. Surg Neurol Int. 11:264.
[Crossref] [Google Scholar] [PubMed]
- Teramoto S, Tsunoda A, Kawamura K, Sugiyama N, Saito R, et al. (2018) Malignant sundural hematoma associated with high grade meningioma. Surg J. 91-95.
[Crossref] [Google Scholar] [PubMed]
- Wang HC, Wang BD, Chen MS, Li SW, Chen H, et al. (2016) An underlying pathological mechanism of meningiomas with intratumoral hemorrhage: Undifferentiated microvessels. World Neurosurg. 319-327.
[Crossref] [Google Scholar] [PubMed]
- Popovic EA, Lyons MK, Scheithauer BW, Marsh (1994) Mast cell-rich convexity meningioma presenting as chronic subdural hematoma: A case report and review of literature. Surg Neurol. 42:48
[Crossref] [Google Scholar] [PubMed]
Citation: Ong-Lingan MC (2023) Atypical Meningioma with Chronic Subdural Hematoma: A Case Report. Neurooncol. 8:001.
Copyright: © 2023 Ong-Lingan MC. This is an open-access article distributed under the terms of the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and
source are credited.