Research Article - (2023) Volume 9, Issue 2
Astigmatism Correction with Limbal Relaxing Incisions with Cataract Surgery and IOL Implantation Compared to Cataract Surgery and IOL or Toric IOL Implantation Alone
Alexander Miller1*,
Matthew Hirabayashi1,
Timothy Ritchie1,
Eli Pratte1,
Samuel Barry1 and
Jella An2
1Department of Ophthalmology, University of Missouri, Columbia MO, USA
2Department of Ophthalmology, Johns Hopkins University, Baltimore, USA
*Correspondence:
Alexander Miller, Department of Ophthalmology, University of Missouri,
Columbia MO,
USA,
Email:
Received: 14-Sep-2022, Manuscript No. IPJECS-22-14301;
Editor assigned: 16-Sep-2022, Pre QC No. IPJECS-22-14301 (PQ);
Reviewed: 30-Sep-2022, QC No. IPJECS-22-14301;
Revised: 14-Jan-2023, Manuscript No. IPJECS-22-14301 (R);
Published:
03-Feb-2023, DOI: 10.21767/2471-8300-9.2.022
Abstract
Purpose: To determine the astigmatism correcting potential of Limbal Relaxing Incisions (LRI) at the time of cataract surgery compared to cataract surgery with monofocal or toric IOLs. Design: Retrospective chart review. Subjects, participants and/or controls: 150 eyes from patients who underwent cataract surgery and either: LRI with monofocal IOL implantation, toric IOL implantation or monofocal IOL implantation.
Methods: A retrospective review of adult patients who underwent cataract surgery between 12/05/17 and 05/11/21. To compare change in astigmatism between the groups, pre-operative keratometry values were compared to postoperative manifest refractions. Astigmatism was plotted on double angle plots for further visualization. Main outcome measures: The primary outcome measure was achievement of postoperative astigmatism of <1.00 D.
Results: 44% (22/50) of LRI eyes and 80% (40/50) of toric eyes achieved a residual postoperative astigmatism of <1.00 D (P<.002). Similarly, 16% (20/50) of LRI eyes and 40% (20/50) of toric eyes achieved a residual postoperative astigmatism of <0.50 D (P<.014). Mean astigmatism resolution in our sample was 1.12 D ± 0.76 D in the LRI group, 0.53 D ± 0.43 D in the toric group and 0.73 ± 0.61 in the standard IOL group.
Conclusion: The toric group resulted in lower rates of post-operative astigmatism as compared to the LRI group. The standard IOL group had a low rate, but they also had a low rate pre-operatively.1
Keywords
Cataract surgery; Astigmatism; Implantation alone; Toric intraocular lens
Introduction
Residual astigmatism following cataract surgery greatly reduces a patient’s uncorrected visual potential and quality of life in multiple ways. Therefore, it is important for cataract surgeons to treat astigmatism at the time of surgery to ensure the best possible refractive outcomes. There are currently multiple ways to minimize astigmatism at the time of cataract surgery including limbal relaxing incisions, intentional wound placement and toric Intra Ocular Lens (IOL) implantation. Limbal Relaxing Incisions (LRI) are a cost-effective method to reduce postoperative astigmatism by placing superficial cuts in clear cornea near the limbus to allow reduction of astigmatism up to 1.5D. While not proven to be superior to toric IOL placement, it is comparatively inexpensive and valuable when toric IOLs are not an option for implantation. Toric lenses are capable of correcting large amounts of astigmatism through cylindrical correction incorporated into the IOL itself. Despite significant improvement of quality of vision, the higher initial cost of toric IOLs precludes implantation in many patients. Toric IOL’s have demonstrated superiority to LRI in terms of ability to resolve astigmatism to within 0.5 D and the data supports that LRI tends to under correct astigmatism. Additionally, toric IOLs may produce more consistent and longer lasting results than LRI. Toric IOL implantation is also effective when combined with LRI in cases of astigmatism >2.50D. Cataract surgery by phacoemulsification and IOL implantation is often performed with small wounds of 2.5 mm or under and this has consistently shown to have a minimal effect on postoperative corneal astigmatism. Due to the major economic benefit of LRI as well as its value in resource-scarce regions, additional studies comparing LRI and toric IOLs to monofocal IOLs would help further clarify the utility and scope of use for LRI. In this study, we sought to quantify and compare the astigmatic change following LRI, toric IOLs and cataract extraction with standard monofocal IOLs [1-5].
Materials and Methods
Data was collected for three groups of patients: Cataract extraction with LRI and standard IOL implantation, cataract extraction with toric IOL and cataract extraction with standard IOL implantation. In total, 150 eyes from 114 patients who had cataract surgery between 12/5/17 and 5/11/21 were included in the study. The patients had no additional procedures performed with the exception of Kahook dual blade goniotomy, which was shown not have a significant astigmatic effect compared to that of cataract surgery alone. Approval from the Institutional Review Board (IRB) of the university of Missouri was obtained. The study adhered to all tenets of the declaration of Helsinki. In order to compare change in astigmatism induced by the surgeries, we collected preoperative keratometry values from the biometry and compared them to postoperative manifest refractions after minimum 1 month postoperatively to allow sufficient healing. Manifest or auto refraction data was collected at 1 month. Astigmatism was plotted on double angle plots for further visualization and analysis [6-9].
Outcome Measures
The primary outcome measure was achievement of postoperative residual astigmatism of <1.00 D or <0.50 D. This was compared between the LRI and toric groups. We also reported the mean absolute amount of surgically induced astigmatism. For this, we compared the LRI group to the cataract extraction with standard IOL implantation alone group and the toric group to the cataract extraction with standard IOL implantation alone group. We also report the pre and post-operative astigmatism values for each group to subjectively assess change and benefit [10-12].
Surgical Technique
All the cataract extractions in this study were performed in a standard manner with a 2.4 mm temporal near clear-corneal wound. LRI axis and length was calculated using the Donne field formula and performed using a diamond keratome at 550 micron depth, paired unless one of the arc overlaps the temporal wound, in which case the nasal arc length was doubled up to the maximum 60°. Steep meridian was based on preoperative corneal topography. Toric axis was calculated using a Barrett true K formula and the pre-determined surgeon factor of 0.2° at 180° or 0° [13-15].
Data Analysis
The mean surgically induced astigmatism of the LRI and toric group were compared to the standard IOL group with student’s t-tests. All statistical tests were 2-tailed with alpha=0.05. Statistical analysis was conducted in IBM SPSS Statistics for Windows, version 24 (IBM Corp., Armonk, N.Y., USA). Double angle plots were used for baseline and postoperative astigmatism visualization using the plotting tool created.
Results
Baseline patient and eye data was comparable between groups except for the amount of pre-operative astigmatism which expectedly was higher in the toric group (Table 1).
| Subject-Level Parameters |
LRI (n=40) |
Toric IOL (n=38) |
Standard IOL (n=36) |
P-value* |
| Age (yr), mean ± SD |
69.9 ± 10.6 |
69.1 ± 10.3 |
68.6 ± 9.6 |
0.736 |
| Gender, % (n) |
| Male |
47.5 (19) |
39.5 (15) |
41.7 (15) |
0.475 |
| Female |
52.5 (21) |
60.5 (23) |
58.3 (21) |
|
| Ethnicity, % (n) |
| Caucasian |
87.5 (35) |
92.1 (35) |
75% (27) |
0.503 |
| Other* |
12.5 (5) |
7.9 (3) |
25% (9) |
| Eye-level parameters |
LRI (n=50) |
Toric IOL (n=50) |
Standard IOL (n=50) |
P-value |
| Pre-op astigmatism (D), mean ± SD |
1.64 ± 0.70 |
1.91 ± 0.43 |
0.73 ± 0.61 |
0.022 |
| Pre-op axis (°), mean ± SD |
87.4 ± 47.3 |
97.9 ± 47.3 |
72.7 ± 44.8 |
0.27 |
| Note: *Comparisons between LRI and Toric group Abbreviations: LRI: Limbal Relaxing Incisions; IOL: Intraocular Lens; SD: Standard Deviation |
Table 1: Baseline demographic and astigmatism data.
We found that the 44% (22/50) the LRI group achieved a residual postoperative astigmatism of <1.00 D compared to 80% (40/50) the toric group (P<.002). Similarly, 16% (20/50) of the LRI group achieved a residual postoperative astigmatism of <0.50 D compared to 40% (20/50) the toric group (P<.014) (Table 2).
| |
LRI |
Toric |
P value |
| Proportion Achieving <1.00 D, |
44% (22/50) |
80% (40/50) |
<.002* |
| Proportion Achieving <0.50 D, % (n) |
16% (8/50) |
40% (20/50) |
<.014* |
| |
LRI |
Toric |
Standard IOL |
| Post-op Astigmatism (D), mean ± SD |
1.12 ± 0.76 |
0.53 ± 0.43 |
0.49 ± 0.38 |
| Surgically Induced Astigmatism (D), mean ± SD |
0.52 ± 0.84 |
1.38 ± 0.77 |
0.25 ± 0.68 |
| Note: Abbreviations: CE/IOL=cataract extraction with standard IOL implantation. |
Table 2: Comparison of astigmatism before and after LRI, Toric and standard IOL alone.
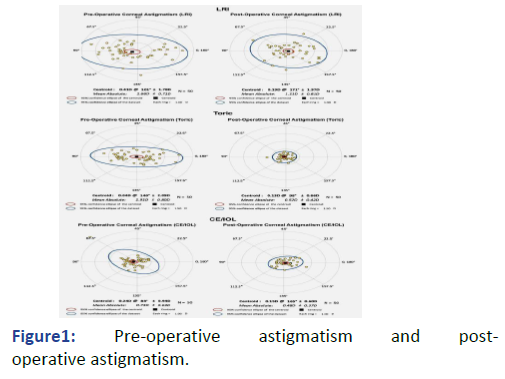
Double Angle Plots
The double angle plots are presented below for pre and post-operative astigmatism. The ring scale is adjusted to 1.50 D for the toric group due the greater preoperative astigmatism compared to the other groups. All groups experienced an overall reduction in mean absolute astigmatism. As calculated above, the LRI group experienced around a 0.50 D reduction in astigmatism. The toric group experienced a significant reduction in astigmatism. The standard IOL group did not have a clinically significant change in astigmatism (Figure 1).
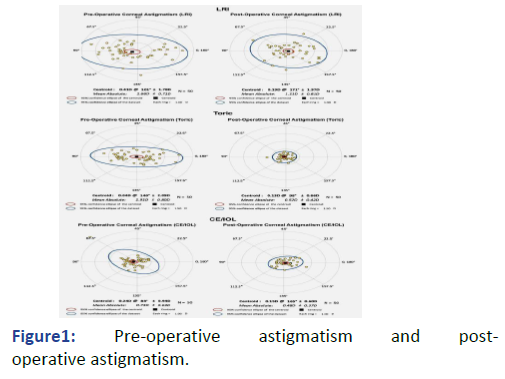
Figure 1: Pre-operative astigmatism and post-operative astigmatism.
Discussion
Although the LRI group had lower rates of achieving low postoperative residual astigmatism compared to toric IOLs, nearly half of the eyes had postoperative astigmatism <1.00 D. The goal of astigmatism reduction is certainly dependent on individual circumstance, but we found the LRI in our sample reduced an average of around 0.50 D. Since residual astigmatism as little as 1.00 D can adversely affect a patient’s postoperative vision, LRI may be of particular benefit to patients in the ~1.00 D range. While there is evidence that toric IOLs have the potential to result in less patient cost throughout their lifetime (e.g., due to spectacle independence etc.), many cannot afford the cost of a premium lens. While highly variable, toric IOLs can cost patients around $1,500-$2,000 per eye. At our institution, patients were not charged for LRI [16-19].
Conclusion
For patients with greater than 1.50 D of astigmatism, a more careful cost, risk and benefit conversation is likely necessary with patients. This study has several limitations including its retrospective nature. First, the preoperative standard IOL group had lower rates of astigmatism, thus lower rates of astigmatism post-operatively. Next, while preoperative keratometry from the IOL biometry provides accurate calculations of corneal astigmatism (especially newer models that can calculate the anterior and posterior cornea), the use of manifest refraction as the post-operative measurement is potentially problematic. Manifest refraction theoretically measures only the corneal component in pseudophakic patients due to removal of lenticular astigmatism and lens tilt astigmatism must be substantial to cause any clinical effects. Regardless, manifest refraction is still subjective in nature so there is the potential of unaccounted confounders from both the patient and refractionist. Despite these limitations, our findings are logically reasonable and consistent with existing studies and to our knowledge this is the first study to quantify and compare astigmatism resolution LRI, toric and standard IOLs. An inexpensive procedure, LRI may have the potential of resolving low levels, but visually significant, amounts of astigmatism especially in the ~1.00 D range. It is possible that in these eyes with low amounts of cylinders surgeons and patients may not feel toric is financially justified could benefit the most from LRI.
References
- Wolffsohn JS, Bhogal G, Shah S (2011) Effect of uncorrected astigmatism on vision. J Cataract Refract Surg. 37(3):454-460. [Crossref] [Google Scholar] [PubMed]
- Black AA, Wood JM, Colorado LH, Collins MJ (2019) The impact of uncorrected astigmatism on night driving performance. Ophthalmic Physiol Opt. 39(5):350-357. [Crossref] [Google Scholar] [PubMed]
- Amesbury EC, Miller KM (2009) Correction of astigmatism at the time of cataract surgery. Curr Opin Ophthalmol. 20(1):19-24. [Crossref] [Google Scholar] [PubMed]
- Monaco G, Scialdone A (2015) Long-term outcomes of limbal relaxing incisions during cataract surgery: Aberrometric analysis. Clin Ophthalmol. 9:1581-1587. [Crossref] [Google Scholar] [PubMed]
- Lim R, Borasio E, Ilari L (2014) Long-term stability of keratometric astigmatism after limbal relaxing incisions. J Cataract Refract Surg. 40(10):1676-1681. [Crossref] [Google Scholar] [PubMed]
- Visser N, Bauer NJC, Nuijts RMMA (2013) Toric intraocular lenses: Historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes and complications. J Cataract Refract Surg. 39:624-637. [Crossref] [Google Scholar] [PubMed]
- Kaur M, Shaikh F, Falera R, Titiyal J (2017) Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol. 65(12):1301. [Crossref] [Google Scholar] [PubMed]
- Pineda R (2010) Economic evaluation of toric intraocular lens: A short and long-term decision analytic model. Arch Ophthalmol. 128(7):834-874. [Crossref] [Google Scholar] [PubMed]
- Lake JC, Victor G, Clare G, Porfírio GJ, Kernohan A, et al. (2019) Toric intraocular lens versus limbal relaxing incisions for corneal astigmatism after phacoemulsification. Cochrane Database Syst Rev.12(12):CD012801. [Crossref] [Google Scholar] [PubMed]
- Lam DKT, Chow VWS, Ye C, Ng PK-F, Wang Z (2016) Comparative evaluation of aspheric toric intraocular lens implantation and limbal relaxing incisions in eyes with cataracts and ≤ 3 dioptres of astigmatism. Br J Ophthalmol. 100(2):258-262. [Crossref] [Google Scholar] [PubMed]
- Freitas GO, Boteon JE, Carvalho MJ, Pinto RMC (2014) Treatment of astigmatism during phacoemulsification. Arq Bras Oftalmol. 77(1):40-46. [Crossref] [Google Scholar] [PubMed]
- Ouchi M, Kinoshita S (2011) AcrySof IQ toric IOL implantation combined with limbal relaxing incision during cataract surgery for eyes with astigmatism >2.50 D. J Refract Surg. 27:643-647. [Crossref] [Google Scholar] [PubMed]
- Hill W (2008) Expected effects of surgically induced astigmatism on AcrySof toric intraocular lens results. J Cataract Refract Surg. 34(3):364-367. [Crossref] [Google Scholar] [PubMed]
- Yang J, Wang X, Zhang h, Pang Y, Wei RH (2017) Clinical evaluation of surgery-induced astigmatism in cataract surgery using 2.2 mm or 1.8 mm clear corneal micro-incisions. Int J Ophthalmol. 10(1):68-71. [Crossref] [Google Scholar] [PubMed]
- Yang J, Wang X, Zhang h, Pang Y, Wei RH, Hirabayashi M, et al. (2020) Effect of excisional goniotomy with the Kahook Dual Blade (KDB) on surgically induced astigmatism. Clin Ophthalmol. 4:4297-4303. [Crossref] [Google Scholar] [PubMed]
- Sivak JG, Kreuzer RO, Hildebrand T (1985) Intraocular lenses, tilt and astigmatism. Ophthalmic Res. 17(1):54-59. [Crossref] [Google Scholar] [PubMed]
- Abulafia A, Koch DD, Holladay JT, Wang L, Hill W (2018) Pursuing perfection in intraocular lens calculations: IV. Rethinking astigmatism analysis for intraocular lens-based surgery: Suggested terminology, analysis and standards for outcome reports. J Cataract Refract Surg. 44(10):1169-1174. [Crossref] [Google Scholar] [PubMed]
- Ouchi M (2014) High-cylinder toric intraocular lens implantation versus combined surgery of low-cylinder intraocular lens implantation and limbal relaxing incision for high-astigmatism eyes. Clin Ophthalmol. 8:661-668. [Crossref] [Google Scholar] [PubMed]
- Leon P, Pastore M, Zanei A (2015) Correction of low corneal astigmatism in cataract surgery. Int J Ophthalmol. 8(4):719-724. [Crossref] [Google Scholar] [PubMed]
Citation: Miller A, Hirabayashi M, Ritchie T, Pratte E, Barry S, et al. (2023) Astigmatism Correction with Limbal Relaxing Incisions with Cataract Surgery and IOL Implantation Compared to Cataract Surgery and IOL or Toric IOL Implantation Alone. J Eye Cataract Surg. 9:22
Copyright: © 2023 Miller A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.