Introduction
While the prevalence of obesity in children and adolescents aged 2-19 in the United States has remained stable at about 17% since 2003 [1] childhood obesity continues to be an area of significant concern. Obesity rates tend to be highest among children in families who function at or below the poverty threshold [2]. While studies have found higher than average prevalence of obesity in urban youth [3], comparative studies indicate that children residing in rural areas also run higher than average risk of obesity [4,5] with children in rural areas having up to 30% greater chance of being overweight or obese than children in non-rural areas even after adjustments for sociodemographic, health, diet and exercise [6].
Not only is the prevalence of obesity a concern, but the consequences of childhood obesity are serious with strong links to a number of health conditions that occur during childhood and extend into adulthood. Children who are overweight have a higher likelihood of having type 1 diabetes and those who are obese are more likely to have asthma, high blood pressure, and type 2 diabetes during their youth than children within normal weight limits [3,7] Childhood obesity is also linked to health conditions of adulthood that contribute to early morbidity and mortality including cardiovascular disease, type 2 diabetes mellitus, fatty liver disease, sleep apnea, asthma, infertility, and certain cancers [8].
Childhood obesity likely contributes to poor long-term health outcomes for several reasons, one of which is the fact that excessive body mass impairs children’s ability to be physically active. Overweight children demonstrate lower movement skill proficiency than their normal weight counterparts [9]. Weight status has been shown to be inversely correlated with development of fundamental motor skills and physical literacy, i.e., a child’s ability to move confidently and with control in a wide range of physical activity situations. Such deficits may affect children’s ability, confidence and motivation to be physically active [10]. Children who don’t exercise at all have 62% higher odds of obesity than children who exercise 5 or more days per week [11].
In addition to obesity’s negative relation with physical activity, childhood obesity is associated with increased rates of psycho-social problems and poor quality of life [12]. The presence of obesity is also inversely correlated with children’s perceived health-related quality of life with the strongest correlations present in females and children living in urban areas [13]. Specifically, female children are more likely to report poor general health and functional limitations in health related quality of life than their male counterparts [14]. Children living in urban areas who are overweight are more likely to be dissatisfied with body size, attempt to lose weight, and have lower self-esteem than children of healthy weight [15]. Strong links have been established between obesity and the presence of chronic stress often associated with many facets of urban living [16,17].
Childhood obesity’s negative impact on development and long term consequences precipitate the need to improve efforts to prevent and reduce obesity in children, particularly those residing within under-resourced areas including urban centers. While the prevalence of obesity in the United States has been extensively studied and the correlations between obesity and motor performance and quality of life have been established, there remains a need to further investigate the relationship of obesity with specific aspects of motor performance and perceived quality of life, especially in an urban youth population. A better understanding of the extent to which weight status influences the specific areas of motor performance and quality of life may provide foundational knowledge upon which youth programs may be developed. To address the deficits in the literature, we designed a study to answer the following questions:
How does the urban youth BMI data of our sample compare to national norms?;
Are there significant differences in motor performance and perceived quality of life based on BMI?;
Are there gender differences impacting the relationships of BMI with motor performance and perceived quality of life?; and
What are the correlations among BMI, motor performance, and perceived quality of life?
We hypothesize that gross motor performance and perceived quality of life will be inversely correlated with BMI, with significantly better performance and more positive responses in those children with healthy weight than those who are overweight or obese.
Methods
A cross-sectional descriptive study was conducted to answer the research questions using a convenience sample of urban youth participating in a health promotion program in a Hartford, CT public school. The community-campus partnership aimed to intentionally engage youth, college students, and community partners through shared learning in the following four areas; nutrition education, physical activity, life skill development, and academic enrichment. An information sheet describing the project as approved by the university’s institutional review board was sent home with each participant, and parents/guardians were instructed to sign and return the form if they did not agree for their child to be enrolled in the study.
Participants
All study participants were enrolled in the participating public school whose catchment area was exclusively from the surrounding urban district. Data from a sample of 130 out of the 177 participants could be used for analysis; 45 participants were eliminated because birthdate information was not available and 2 children were not included because they were classified as underweight by Center for Disease Control standards and were, therefore, not in the healthy weight range. Our final sample of 130 students consisted of slightly more females (n=70; 54%) than males (n=60; 46%) ranging in age from 7-14 years with the majority (61%) being 9–11 years of age. Failure of all subjects to perform every test measure was encountered due to time constraints and children’s unwillingness to participate with certain tasks.
Instruments
Anthropometric measurements of height and mass were taken and used to determine participants’ body mass index (BMI) and BMI percentiles factoring age and gender as specified by the CDC (2). The Center for Disease Control (CDC) classifies children in the 5th -85th percentile of body mass index as normal, healthy weight. Those below the 5th percentile are classified as underweight, those in the 85th-95th percentile are overweight, and those above the 95th percentile are obese.
Motor performance was measured using components of the Bruininks-Oseretsky Test – 2nd Edition (BOT-2), a valid and reliable measure of motor abilities in children 4-21 years of age [18]. Speed and agility were measured using single-leg stationary hop, single-leg side hop, double-leg side hop, and shuttle run as described in the BOT-2 protocol. Strength tests consisted of push-ups, sit-ups, wall-sits and V-ups (trunk extension).
Additionally, the children’s perceived quality of life was measured using the Pediatrics Quality of Life Questionnaire (PedsQL), a valid and reliable measure for children ages 2-18 [19]. The PedsQL, administered as a clinician interview, considers health, home life, school performance and physical activity by asking children if they never, rarely, sometimes, often or always have trouble performing a variety of activities including walking, running, playing sports, lifting, bathing, and doing chores. The questionnaire also asks if children experience aches and low energy. In addition, children were asked to report their thoughts on participating in other sports.
Trained faculty, undergraduate, and graduate students delivered tests following the protocols recommended by the BOT-2 and PedsQL. Testing was conducted in stations with groups of 1-5 students. Participants’ performance in the strength station was video recorded to allow grading by trained personnel following the BOT-2 guidelines.
Statistical analysis
Data analyses were accomplished using SPSS-Version 22 with a priori level of 0.05. The percentage of obese children in our sample was compared to national norms, as defined by the CDC, using an independent sample t-test. Analyses of motor performance utilized raw instead of standardized scores of BOT-2 components to address the research question of how weight, not age may affect motor performance with greater specificity than conversion to standard scores would allow. Pearson correlations were used to evaluate the relationship between BMI and motor performance measures while Spearman correlations were used to explore the relationship between BMI and PedsQL responses. Variance (r2) was calculated to explore the contribution of children’s BMI on BOT-2 results and PedsQL responses.
Separate two-way between subject analyses of variance (ANOVA) were performed to determine if any significant differences existed in motor performance and perceived quality of life responses based on BMI percentile categories (normal and overweight/obese) and gender. Additionally, confidence intervals were calculated for descriptive purposes.
Results
Using classifications defined by the CDCs, the overall frequency of children with healthy BMI percentiles in our sample was 61.5%. Those considered to be overweight made up 7.7% and those who were obese were 30.8%.
An independent t-test indicated that the percent of children who were obese in our sample was significantly higher than the published national norms (18% in children ages 6-11 and 21% in children ages 12-19) [2].
Overweight and obese groups were combined in subsequent analyses to represent children who were outside of the upper limits of healthy weight.
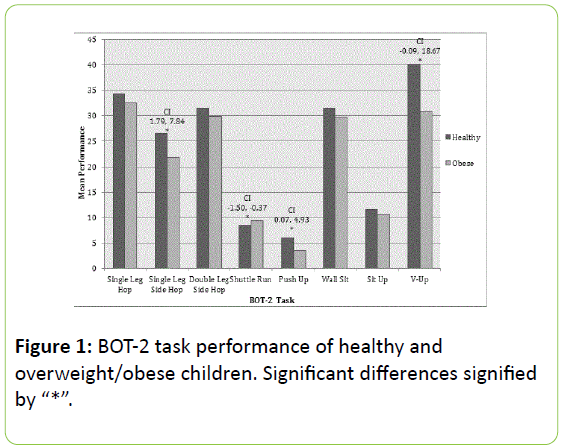
When considering the relationship of BMI with motor performance, analyses indicated that statistically significant differences were present between BMI categories in single leg side-hop (p=0.002, CI [1.79, 7.84]), shuttle run (p=0.001, CI [-1.50, -0.37]), push up (p=0.44, CI [0.07, 4.93]), and v-up (p=0.05, CI [-0.09, 18.67]), with lower performance associated with children categorized as overweight/obese (Figure 1).
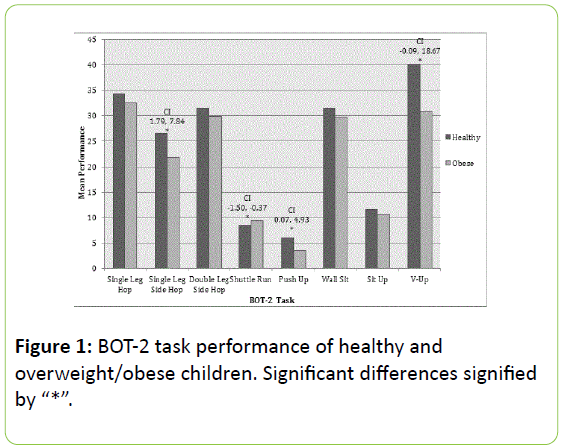
Figure 1: BOT-2 task performance of healthy and overweight/obese children. Significant differences signified by “*”.
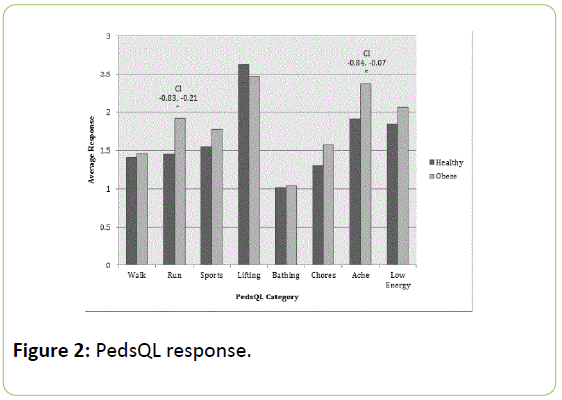
Significant differences in perceived quality of life responses were also present with respect to BMI in children’s report of difficulty running (p=.011, CI [-0.83, -0.21]) and presence of aching ((p=.017, CI [-0.84, -0.07]) such that overweight/obese children reported more negative responses (Figure 2).
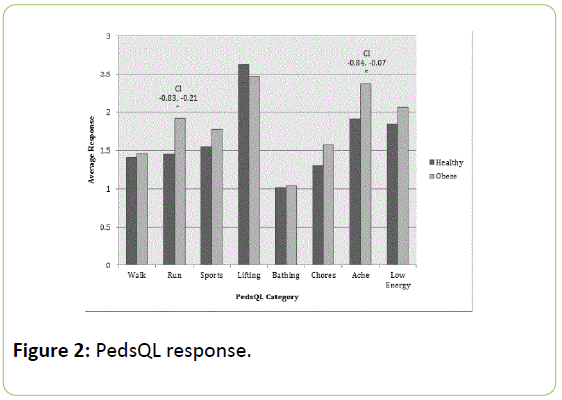
Figure 2: PedsQL response.
When considering the influence of gender on BOT-2 task performance, significant difference was found only in shuttle run performance. No gender effects were evident in PedsQL responses (p>0.05). There were no significant interactions between gender and BMI in any other dependent measures (p>0.05).
In terms of BOT-2 performance, BMI percentile was significantly correlated with single leg side-hop and shuttle run such that as BMI percentile increased performance worsened (Table 1).
| BOT-2 Item (n) |
p value |
Variance (r2) |
Single-leg Hop
(n=102) |
0.08 |
0.03 |
Single-leg Side Hop*
(n=103) |
0.002 |
0.1 |
Double-leg Side Hop
(n=102) |
0.13 |
0.02 |
Shuttle Run*
(n=118) |
0.02 |
0.05 |
Push Up
(n=90) |
0.33 |
0.01 |
Wall Sit
(n=105) |
0.92 |
0 |
Sit Up
(n=98) |
0.73 |
0.001 |
| V-Up (n=100) |
0.13 |
0.02 |
Table 1: Correlation between BMI percentile and BOT-2 performance.
Within quality of life responses, BMI percentile was significantly correlated with the participant’s report of difficulty running and their choice to participate in other physical activity (Table 2).
| QOL Response (n) |
p value |
Variance (r2) |
| Walking (n=130) |
0.52 |
0 |
| Running*(n=130) |
0.02 |
0.04 |
| Sports (n=129) |
0.06 |
0.03 |
| Lifting (n=129) |
0.89 |
0 |
| Bathing (n=128) |
0.34 |
0.01 |
| Chores (n=129) |
0.31 |
0.01 |
| Ache (n=129) |
0.81 |
0.02 |
| Low Energy (n=129) |
0.08 |
0.01 |
| Choice to participate in other physical activity*(n=129) |
0.02 |
0.04 |
Table 2: Correlation between BMI percentile and quality of life response.
As a means of exploring possible contributing factors, we additionally considered correlations within the participants’ responses to items represented on the PedsQL. Children’s report of experiencing ache was significantly correlated (p< 0.05) with six other PedsQL responses including difficulty walking more than a block (p=0.049, r2=0.03), difficulty running (p=0.001, r2=0.10), difficulty engaging in sport activities (p=0.01, r2=0.05), difficulty bathing (p=0.044,r2=0.03), difficulty helping with household tasks (p=0.015, r2=0.05), and lack of energy (p=0.001, r2=0.13).
Children’s report of having low energy was significantly correlated with participants’ responses on six other quality of life items including difficulty walking more than a block (p=0.002, r2=0.07), difficulty running (p=0.003, r2=0.07), difficulty engaging in sport activities (p=0.002, r2=0.07), difficulty lifting (p=0.036, r2=0.03), aching (p=0.001, r2=0.13), and participation in other physical activity (p=0.02, r2=0.04).
Discussion
Approximately 30% of children in our sample were categorized as obese, and a total of 38.5% were considered overweight or obese. This prevalence of childhood obesity within our sample is significantly greater than the national average of 17% as defined by the CDC [2]. Although various studies have identified higher obesity rates in children living in rural areas than non-rural areas [4,20], other evidence supports our findings demonstrating higher than average levels of obesity in urban youth populations [8,21]. Findings from this study reinforce the concern that childhood obesity is a major health issue, especially in urban youth populations that frequently lack resources, green spaces, adult supports, and consistent access to opportunities for physical activity, and reinforce the national concern about childhood obesity and its health threat.
Healthy students outperformed the overweight/obese children in every motor performance measure tested, with significantly greater performance in the single-leg side hop, shuttle run, push-up, and v-up tasks by those with less body mass. These tasks fall specifically in the ‘speed and agility’ and ‘strength’ areas of the BOT-2. Our conclusion that children of healthy weight more effectively complete motor performance tasks, concurs with findings of Lubans et al. [10] indicating that fundamental motor skills are positively associated with increased physical activity and inversely related to weight status in children. Children who do not develop mastery of fundamental motor skills may choose to opt out of the few opportunities to be physically active (i.e., physical education class) due to perceptions about lack of skill and diminished confidence, which contribute to poor physical literacy. This is especially important to consider since motor performance in childhood and adolescence augments health related physical fitness in adulthood and may enhance development of longterm health related outcomes [10].
Programs embedded in educational settings have provided sustainable interventions to help address childhood obesity in some cases [3]. Those programs that have attained some level of success have delivered culturally sensitive interventions relating to both nutrition and physical activity [3,11,22]. The findings of this study indicate that attention to the specific components of physical performance, i.e., strength, speed, and agility, may also improve the likelihood of success. Addressing strength, speed, and agility may give children the foundational building blocks on which to advance motoric skills and thus increase their ability to engage in higher level physical activities. Greater engagement in physical activity is associated with diminished likelihood of obesity [11].
In addition to physical performance, differences existed in children’s responses to quality of life questions based on their body mass. Overweight and obese children consistently reported higher values on the PedsQL in seven out of the eight items, indicating these children report significantly greater difficulty with running, and a greater presence of aching and pain. The results of this study are in agreement with Wynne’s conclusion that BMI has been found to have a weak inverse relationship with health related quality of life [13].
Our exploration of the effect of gender on motor performance yielded no evidence of effect with the exception of shuttle run, in which males were faster than females. However, when gender and BMI were considered together, there were no significant differences in any of the physical performance measures. Despite paucity in the literature evaluating gender and weight status concurrently, comparable findings stating similar performance curves in motor performance are found between genders until puberty [21]. Lack of gender differences in the current study, may be associated with the fact that the majority of our subjects were in the pre-adolescent age range.
With respect to quality of life responses, no gender effect was found. This finding is contrary to those of Swallen et al. [14] that stated females were more likely to report poor general health and functional limitations in health related quality of life. This study’s sample age and demographic characteristics may play a role in this difference in research findings. The current study findings support that interventions to improve children's’ quality of life should not be targeted to a specific gender, but rather provided to all children.
While it is important to identify the presence of significant differences in specific areas of motor performance based on healthy and non-healthy BMI, it is equally important to attempt to determine the extent of BMI’s influence on performance. To further investigate the impact of BMI on motor performance we explored the correlation between BMI percentile and BOT-2 task performance and calculated the variance in performance accounted for by BMI. Significant correlations were found only in single leg side hop and shuttle run. While these correlations were significant, the variance is relatively low, suggesting a weak contribution from BMI on the performance of these tasks.
To help explain possible factors that may influence the low variance in motor performance and quality of life accounted for by BMI and gender, we further investigated the correlations between certain PedsQL responses. The two particular responses we focused on were ‘ache’ and ‘low energy’ as they had the highest correlation with performance related items. The results indicated a direct correlation between children’s report of experiencing both ache and lowenergy with six other PedsQL answers. In addition, these two PedsQL responses also correlated with each other and had common correlations with walking, running, and participation in sports. These results demonstrate influences outside of BMI that may impact a child’s ability to complete motor performance tasks. There are known links between stress and report of pain in children [23]. The findings of this study are in concert with others studies that have found that children undergoing chronic stress, especially those in urban areas, have greater risk of obesity [16,17]. The ache they feel during motor tasks, their perceived difficulty of the task, and their willingness and ability to participate in sports and physical activity are among other elements beyond BMI that may affect motor performance.
This brings forth important and troubling questions that can hopefully be addressed with future research. Are children who are predisposed to experiencing pain failing to perform an adequate amount of physical activity resulting in obesity? Or, are children who are predisposed to being obese more likely to experience pain resulting in low energy and subsequent inactivity? This study demonstrated that children who clearly experience aches and pain are more likely to report difficulty performing functional activities and are more likely to have compromised performance of foundational motor skills. This gives rise to a causal question of whether children fail to exercise because they are predisposed to experiencing pain or are they experiencing pain because they are already obese? The continued concern surrounding childhood obesity in the United States, may prompt future research that explores the links between pain, physical activity, and obesity in children.
Strengths of this study include the relatively large sample size and the use of valid and reliable measures, BOT-2 and PedsQL administered by trained researchers. However, there were several limitations associated with large-scale field research involving youth participants. The inherent character of any youth population posed a challenge in that children may not attend or adhere completely to directions or exert maximal effort. Constraints of school scheduling also posed a challenge to data collection. Despite these limitations, this study gives an accurate portrait of urban youth’s performance on physical measures and report of perceived quality of life and explores the relationships of these measures with anthropometric factors. It also provides direction for future research that could include longitudinal studies of how children's pain, low energy, and other quality of life responses change as they get older and weight status changes. Research could also look at the hereditary connection between pain, energy levels, obesity and physical activity to determine the extent of the variables’ influence on each other.
In addition to research recommendations, these study findings can also be used as foundations for developing optimal intervention strategies. Management of weight is accomplished through balancing an appropriate nutritional intake and expending energy through physical activity. Programs aimed at encouraging children to exercise in a safe and invigorating manner with a variety of activities may help decrease pain and increase energy levels with potential prolonged health benefits. While some school based programs have been shown to be successful in reducing BMI [22,24], others have not had long lasting success [25,26]. Research supports programs that address the “whole child” and family centered approaches to promote health [22]. The findings of this current study indicate that consideration of children’s perceived discomfort and energy level is warranted when creating comprehensive programs to address obesity. Perhaps including stress and pain management into the programming may optimize success of such programs.
While further research needs to be conducted in an effort to answer the important causal questions, it’s also imperative that more immediate measures be taken to reverse the increasing trend of obesity in today’s urban youth. Health care professionals in conjunction with educational systems may play an important role in decreasing childhood obesity rates. Efforts to ensure all children acquire mastery of fundamental motor skills are essential for children to be physically active during childhood and through adulthood. Educational programs regarding weight management and nutrition implemented in urban school systems may promote children’s healthy lifestyles. Perhaps the addition of pain management strategies in these programs may help to improve children’s motor performance, increase their engagement in exercise, and positively influence their perceived quality of life, especially as it relates to physical activities. Programs such as these may help guide children in the direction towards optimal health, thus decreasing the odds of developing a myriad of health-related conditions that will affect them as children and into their futures as adults.
We would like to thank the children, their parents, and all the staff who made this project possible.
References
- CL Ogden, MD Carroll, BK Kit, KM Flegal (2014) Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 311: 806-814.
- Childhood Obesity Facts (2015) Centers for disease control and prevention.
- M Trent, JM Jenning, G Waterfield, LM Lyman, H Thomas, et al. (2009)Finding targets for obesity intervention in urban communities:School-based health centers and the interface with affected youth.J Urban Health; Bulletin of the NY Acad Med 86: 571-583.
- AM Davis, KJ Bennett, C Befort, N Nollen (2011) Obesity and related health behaviors among urban and rural children in the United States; Data from the national health and nutrition examination survey 2003-2004 and 2005-2006.J Ped Psych 36: 669-676.
- JA Johnson, AM Johnson (2009) Urban-rural differences in childhood and adolescent obesity in the United States:A systematic review and meta-analysis.Childhood Obesity 11: 233-241.
- J Liu, SJ Jones, H Sun, JC Probst, AT Merchant, et al. (2012) Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity:An urban and rural comparison.Childhood Obesity 8: 440-448.
- LL Liu, JM Lawrence, C Davis, AD Liese, DJ Pettitt, et al. (2010) Prevalence of overweight and obesity in youth with diabetes in USA: the SEARCH for Diabetes in Youth Study.Pediatr Diabetes 11: 4-11.
- Latino Policy Institute (2006) A profile of Latino health in Connecticut: The case for change in policy andpractice.
- DP Cliff, AD Okely, PJ Morgan, JR Steele, RA Jones, et al. (2011) Movement skills and physical activity in obese children. Med &Sci Sports & Ex 43: 90-100.
- DR Lubans, PJ Morgan, DP Cliff, LM Barnett, AD Okely, et al. (2010) Fundamental movement skills in children and adolescents. Sports Med 40: 1019-1035.
- GK Singh, MD Kogan, PC Van Dyck, M Siahpush (2008) Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States:Analyzing independent and joint associations. AEP 18:682-695.
- MH Zeller, HR Roehri, AC Modi, SR Daniels, TH Inge, et al. (2006) Health-related quality of life and depressive symptoms in adolescents with extreme obesity presenting for bariatric surgery.Pediatrics 117:1155-1161.
- C Wynne, C Comiskey, E Hollywood, MB Quirke, K O’Sullivan, et al. (2014) The relationship between body mass index and health-related quality of life in urban disadvantaged children. Qual Life Res 23: 1895-1905.
- KC Swallen, EN Reither, SA Haas, AM Meier (2005) Overweight, obesity, and health-related quality of life among adolescents: The national longitudinal study of adolescent health. Pediatrics 115: 340-347.
- NM Mirza, D Davis, JA Yanovski (2005) Body dissatisfaction, self-esteem, and overweight among inner-city Hispanic children and adolescents. J Adolescent Health 36: 267.e16-267.e20.
- J Black, J Macinko (2010) The changing distribution and determinants of obesity in neighborhoods in New York City, 2003-2007.Am J Epid 171: 765-775.
- S Garasky, SD Stewart, C Gunderson, BJ Lohman, J Eisenmann, et al. (2009) Family stressors and child obesity. SocSci Res 38: 755-766.
- RH Bruininks, BD Bruininks (2005) The Bruininks-Oseretskytest of motor proficiency (2ndedn.). Manual. Circle Pines, MN: AGS Publishing.
- JW Varni, M Seid, PS Kurtin (2001) PedsQLTM 4.0: Reliability and validity of the pediatric quality of life inventory TM Version 4.0 generic core scales in healthy and patient populations. Medical Care 39: 800-812.
- DB Reed, PJ Patterson, N Wasserman (2011) Obesity in rural youth: Looking beyond nutrition and physical activity. J Nutrition Ed Behav 43: 401-408.
- JR Thomas, KE French (1985) Gender differences across age in motor performance: A meta-analysis. Psych Bulletin 98: 260-282.
- S Dawson-McClure, L Miller-Brotman, R Theise, JJ Palamar, D Kamboukos, et al. (2014)Early childhood obesity prevention in low-income, urban communities.J PrevInterv Community 42: 152-166.
- S King, CT Chambers, A Huguet, RC MacNevin (2011) The epidemiology of chronic pain in children and adolescents revisited; a systematic review. Pain 152: 2729-2738.
- JF Sallis, TL McKenzie, TL Conway, Elder JP, Prochaska JJ, et al. (2003) Environmental interventions for eating and physical activity: A randomized controlled trial in middle schools. Am J Prev Med 24: 209–217.
- S Barkin, S Gessell, E Poe, J Escarfuller, T Tempesti, et al. (2012) Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children.Pediatrics 130: 1-12.
- SM Winter, DA Sass DA (2011)Healthy and ready to learn:Examining the efficacy of early approach to obesity prevention and school readiness.JRes Child Ed 25: 304-325.