Keywords
Transfusion guidelines; Intensive care; Patient blood management
Introduction
Appropriate use of blood products is one of the "pillars" identified by the Patient Blood Management approach to reduce the use of blood transfusion and to improve the patient outcome. However, various studies demonstrate that inappropriate use of blood component is still frequently observed and the attitude to overtransfuse patients is very difficult to correct, despite a number of guidelines for the use of blood and blood components have been published by various scientific societies and national health authorities. Australian benchmark studies demonstrated considerable variations of the Packed Red Cell (PRC) transfusion rate among institutions [1,2]. Other recent studies demonstrated overtransfusion and administration of double units as common errors [3,4]. Moreover, despite international guidelines are very clear about a sufficient dosage of plasma, underdosage of plasma seems to be an international phenomenon [4,5]. The reason for these observations remains unclear. Continuous information of physicians involved in transfusion practice and monitoring has been claimed to increase the attention for transfusion practice and associated outcome. Since the complexity of a clinical situation such as in critical care might be a further explanation for the difficulty of guidelines adherence, actual reports about transfusion practice in critical care are wanted.
German transfusion guidelines (German transfusion guidelines [6] and Cross Sectional Guidelines for the Use of Blood and Blood Products [7] are very detailed. Critical illness is covered by sometimes very complex recommendations for the therapy with blood and blood products. They are based by a specific German transfusion law [8]; (First edition in 1998, last updates 2007 and 2009). For better adherence, guideline recommendations suggest a clinical transfusion corridor of situations in more or less detail for every blood product. This setting should provide sufficient support for accurate decisions in transfusion practice.
Despite these detailed support, the national German registry for transfusion errors (“IAKH transfusion error registry”) contains a high percentage of errors with misuse (missing transfusion indication) (citation website of the registry report: https://www. iakh.de/auswertung2013.html), maladherence, or ignorance. The registry exists since 2009 and is fed from voluntary reports [9]. Although a collection bias with this hemovigilance clearly exists, the suspicion arises that in contrast to perfect preconditions transfusion practice among German physicians is poor for unknown reasons. For example, restrictive transfusion strategy is a repetitive error although the majority of physicians are educated about the TRICC trial [10]. Still, after more than a decade, implementation of this knowledge into German clinical practice seems to be very difficult.
To verify this thesis and to assess the underlying causes about the use of blood products, a retrospective analysis in an intensive care unit of a Level 1 university hospital was performed. Years after the publication of the detailed cross sectional guidelines, blood product use in accordance or disrespect of existing guidelines was recorded and evaluated for packed red cells, plasma and platelets. In case of non-alignment to guidelines, specific explanations were requested from ordering physicians.
Methods
Study population
A retrospective chart review was done in a 16-bed-perioperative Intensive Care Unit (ICU) at the University Hospital of Marburg, Germany. During a 12 month period, all data sets from transfused critical ill subjects either with red blood cells (PRCs), Fresh Frozen Plasma (FFP’s) and Platelet Concentrates (PC’s) thoroughly were reviewed or analyzed. Excluded from data analysis were patients on ExtraCorporal Membrane Oxygenation (ECMO) therapy or Intraaortic Balloon Pulsation (IABP) since their transfusion requirements are much higher and probably not addressed by guidelines. Our hypothesis was that blood product use in a German university ICU deviates from guidelines in a considerable percentage (>20%) of administrations.
Data collection, categorization and statistics
Transfused patients were identified by delivery and transfusion documents of the university blood bank. Documentation of transfusion indication was extracted from patient’s charts. Laboratory and clinical data as well as other documentation were extracted both from paper and electronic medical records. Additionally, the responsible ward physician for the respective case was interviewed. For each blood product with unclear indication, the responsible physician’s comment was requested and noted. Indications for each product was compared to given requirements in the cross sectional German guidelines (Querschnitts-Leitlinien (BÄK) zur Therapie mit Blutkomponenten und Plasmaderivaten). They were categorized as follows:
Packed red cells (PRC)
For one unit of red blood cells (PRC, 250-280 ml): 1) Transfusion with a unit of PRC is recommended below a hemoglobin content (Hb) ≤ 6 g/dl (EBM 1+); 2): Hb 6-8 g/dl only in patients with preexistent diseases that limit physiological mechanisms for anemia compensation (EBM 1+) or symptoms of anemia (tachycardia, hypotension, ischemic ST-changes, lactacidosis) (EBM 1+); 3): Hb 8-10 g/dl only with symptoms of anemia (tachycardia, hypotension, ischemic ST-changes, lactacidosis) (EBM 2c); 4): In patients with serious illness such as acute respiratory distress syndrome (ARDS), shock, sepsis, multiple trauma, massive blood loss postoperatively/gastrointestinal (GI) bleedings, ICU physicians considered a liberal transfusion strategy due to ongoing blood loss or active bleeding; 5): No transfusion is recommended above Hb 10 g/dl (EBM 1A). In stable patients, administration of double units without reassessment of the patient’s clinical situation following reception of one unit is considered guideline discordant.
Fresh frozen plasma (FFP)
Transfusion of fresh frozen plasma (FFP) is recommended in following settings: 1) Microvascular bleeding following blood loss 100 ml/min; 2) red cell transfusion of more than 2 PRCs within 15 min; 3) transfusion of more than 4-6 PRC's; 4) If prothrombin time, aPTT and fibrinogen after prolonged blood loss, especially together with microvascular bleeding, are not available within brief; 5) PT ≤ 50%; 6) aPTT ≥ 45 s; 7) Fibrinogen ≤ 1 g/L; 8) indication is not to be found or setting is uncovered by guidelines.
Platelets (PC)
Chapter 2 of the cross sectional guidelines specifies the perioperative indications for platelets: 1) In cardiac surgery at increased postoperative bleeding in stable patients or below a platelet count of 20.000/μl; 2) in case of large and threatening bleedings for prophylaxis of a coagulopathy at <100,000 platelets/ μl; 3) during acute blood loss at <100,000 platelets/μl H g or of requirement of ≥ 1 PRC`s per day (WHO grade 3) 4) indication is not to be found or setting is uncovered by guidelines.
Data was analyzed following collection in an access database by Wilcoxon/Kruskall-Wallis ranked sum test. Significance was set at the alpha level of 5%.
Results
During the study period, 89 patients out of 650 ICU patients in total were transfused with blood products (13.7%). Treated patients were elderly (median 71 years) and originated from general, cardiac or orthopedic-trauma surgery departments. Most patients were admitted from other hospitals or departments critical care units (named “external” in Table 1). According to applied blood products, recipients were categorized in groups derived from the guidelines by the "Bundesärztekammer (German Medical Association) (Table 2 - PRC, Table 3 - FFP, Table 4 - PC).
| Patients (n) |
89 |
|
| Gender m/w (% of transfused) |
49 (55%)/40 (45%) |
| Age (years, median (1/3 quartile)) |
71 (51/78) |
| Height (cm, median (1/3 quartile)) |
170 (165/175) |
| Weight (kg, median (1/3 quartile)) |
75 (70/85) |
| Origin |
| Number of patients (%) |
| Admitted from other hospitals ICU |
34 (38) |
Peripheral wards |
6 (6.7) |
| General surgery |
15 (17) |
Nephrology |
3 (3.4) |
| Cardiac surgery |
14 (16) |
Neurosurgery |
1 (1.1) |
| Orthopedics |
7 (7.9) |
Pneumology |
1 (1.1) |
| Trauma surgery |
6 (6.7) |
Gynecology |
1 (1.1) |
Table 1: Demographic data of transfused subjects.
| Indications |
|
n |
% |
| I |
hemoglobin = 6 g/dl |
1 |
0.4 |
| II |
hemoglobin 6-8 g/dl with risk factors* |
44 |
17.67 |
| III |
hemoglobin 6-80 g/dl with signs of anemic hypoxia** |
34 |
13.66 |
| IV |
hemoglobin 8-10 g/dl with signs of anemic hypoxia** |
117 |
46.99 |
| V |
hemoglobin >10 g/dl in critically ill patients*** |
15 |
6.02 |
| VI |
without indication according to guidelines |
75 |
30.12 |
*Coronary disease, heart failure, cerebrovascular disease
**Physiological transfusion trigger: blood pressure = 100 systolic; tachycardia = 100 bpm; catecholamine demand; lactate = 2 mmol/l and/or
acidosis; cardial ischemic signs: ST-Reduction/Elevations, Angina Pectoris, Arrhythmia)
***Suffering from ARDS, shock, sepsis, multiple trauma, massive blood loss postoperatively / GI bleedings
NOTE: For one request of PRC more than one indication could be chosen!
Table 2: Indications for red blood cells.
| Indications |
n |
% |
| I |
19 |
9.5 |
| II |
23 |
11.4 |
| III |
8 |
4.0 |
| IV |
0 |
0.0 |
| V |
14 |
7.0 |
| VI |
88 |
43.78 |
| VII |
0 |
0.0 |
| VIII |
79 |
39.30 |
NOTE: For one request of FFP more than one indication could be chosen!
I. Blood loss 100 ml/min; II. Substitution requirements of more than
2 PRCs per 15 min; III. Following transfusion more than 4-6 PRC's; IV.
If prothrombin time, aPTT and fibrinogen after prolonged blood loss,
especially at microvascular bleeding, are not available within brief; V. PT
= 50%; VI. aPTT = 45 s; VII. Fibrinogen = 1 g/L; VIII. No indication is given
by the guidelines
Table 3: Indication categories for fresh frozen plasma.
| Indications |
n |
% |
| I |
1 |
3.45 |
| II |
12 |
41.38 |
| III |
11 |
37.93 |
| IV |
9 |
31.03 |
NOTE: For one request of platelets more than one indication could be
chosen!
I. In Cardiac Surgery at increased postoperative bleeding in stable patients
or below a platelet count of 20.000/µl; II. In case of large and threatening
bleedings for prophylaxis of a coagulopathy at <100,000 platelets/µl; III.
In acute blood loss at <100,000 platelets/µl or requirement = 1 PRC`s per
day (WHO grade 3) IV. No indication is given by the guidelines
Table 4: Indication category for platelets.
Packed red cells (PRC)
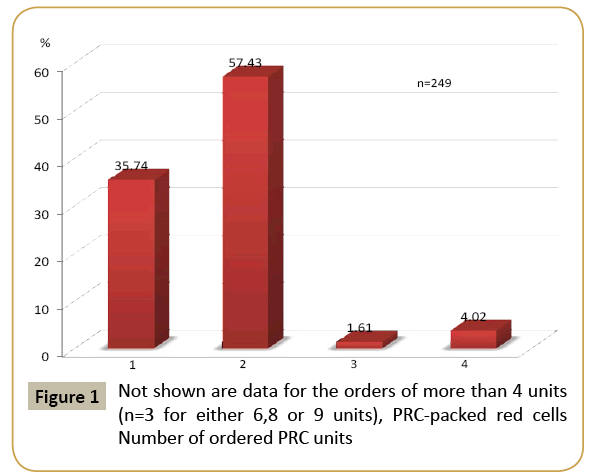
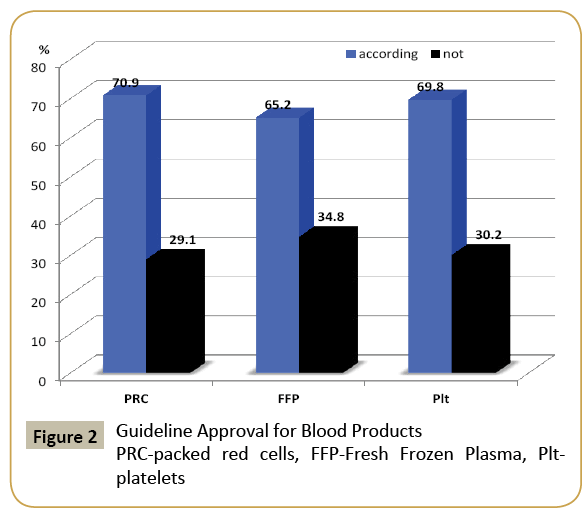
From 89 ICU patients, 78 (87.6%) were transfused with red cells (PRC). Mean transfusion volume per patient was 5.8 +/- 6,6 (mean +/- SD) units of PRC. Almost a third of blood requests at the blood bank (30.12%) and subsequent PRC administrations (29.11%) were off guidelines. Mean hemoglobin levels with or without guideline approval were 82 (78-86) g/L or 88 (84- 96) g/L, respectively. Hemoglobin levels following transfusion with or without indication was 98 g/L or 102 g/L, respectively. Administration of 319 units of PRC was in congruence with guideline recommendations whereas 131 units were not (total n=450). Clinical instability (cardio- and cerebro-vascular) was not associated with an increased transfusion rate (stable n=286, 63.6% vs. instable n=164, 36.4%). Despite similar base line pretransfusion hemoglobin content (84 g/L in both groups, n.s.), subjects with higher comorbidity had higher post-transfusion hemoglobin levels (100 g/L, 75% CI 95-106 vs. 97 g/L, 75% CI 93-104, p=0,0462). Double RBC units were more frequently ordered than any other number of units (Figure 1). Given the mean German acquisition cost of a unit of PRC (average cost 139.68 € [11]), guideline convergent or divergent RBC treatment was associated with estimated cost of 44.557,92 € vs. 18.298,08 €.
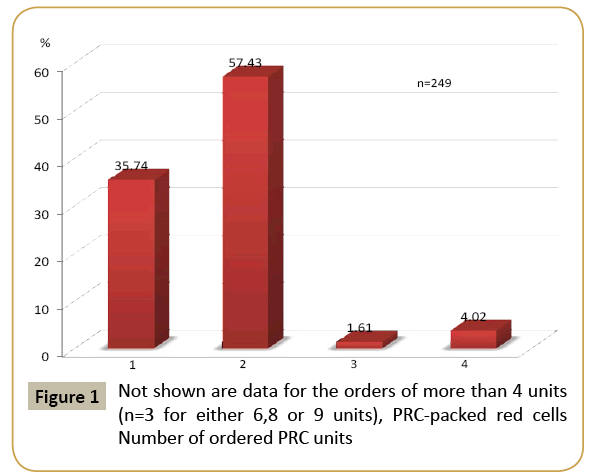
Figure 1: Not shown are data for the orders of more than 4 units (n=3 for either 6,8 or 9 units), PRC-packed red cells Number of ordered PRC units
Fresh frozen plasma (FFP)
Sixty-six recipients were transfused with a mean dose of 14.3 (75% CI 7.7-29.8) ml/kg bw H.A Median 14.29 ml/kg bw or an average of 4 units of FFP. In contrast, the ordered number of units covered a median dose of 7.27 ml/kg body weight. Guideline conformity was given in more than two thirds (n=296 units (69.5%) vs. n=158 units (34.8%)) (Table 3 and Figure 2). Order of a double unit was practiced in 76.12%, whereas single, triple or quadruple unit orders were rare (7.46%, 4.98% or 9.95%, respectively). Pre-transfusion laboratory coagulation variables were unchanged by transfusion (PT (65% vs. 73.5%, respectively), aPTT (46 s vs. 38.5 s) or fibrinogen level (4.7 g/l vs. 4.95 g/l)). Guideline conformity did not change that relation (conform vs. not PT (75% vs. 78.5%), aPTT (50 s vs. 40 s) or fibrinogen level (5.2 g/l vs. 5.3 g/l)). Given the German acquisition cost of a unit of FFP (average cost 52.50 € [11], guideline convergent or divergent FFP treatment was associated with estimated cost of 15.540 € vs. 8.295 €.
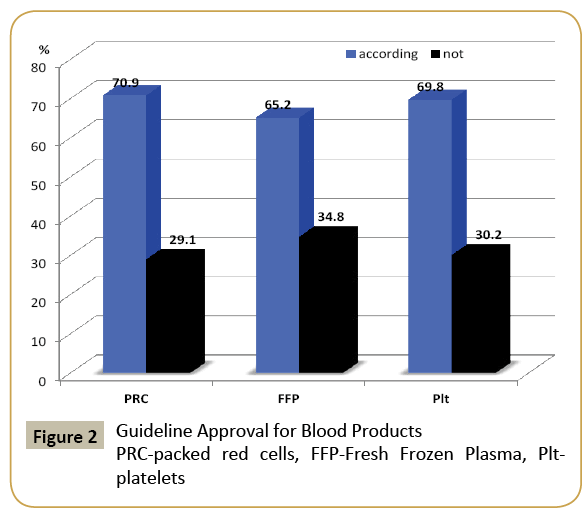
Figure 2: Guideline Approval for Blood Products PRC-packed red cells, FFP-Fresh Frozen Plasma, Pltplatelets
Platelets
Forty-three units of platelets were necessary in 15 patients (mean 2.9 units), in 66% as single unit application (Table 4). Similarly to other blood products, almost a third (31%) of PC applications remained uncovered by guidelines. Low platelet counts (42.5 106/L, 75% CI 30-56 106/L) triggered transfusion in 69.8% of applications. Pre-transfusion platelet counts exceeded 100 106/L (p=0,0404) due to the physician’s assumption of mechanical or drug induced platelet dysfunction. For guideline incongruent use of plasma, 6052.28 € (vs. 13.966,8 €) was spent.
Transfusion triggers
Transfusions triggers and their approval by guideline indication can be seen in Table 5. Controlling for pre (p=0.2263) and post (p=0.0462) transfusion Hb content demonstrated guideline discomform PRC overtransfusion.
| Transfusion laboratory trigger |
With indication |
Without indication |
*p value |
| red blood cell |
|
|
|
| Hb prior to transfusion |
82 g/L |
88 g/L |
|
| Hb following transfusion |
98 g/L |
102 g/L |
|
| |
with risk factors* |
without risk factors |
|
| Hb prior to transfusion |
84 g/L |
84 g/L |
p=0.2263 |
| Hb following transfusion |
100 g/L |
97 g/L |
p=0.0462 |
| Fresh Frozen Plasma |
|
|
|
| |
with indication |
without indication |
|
| PT prior to transfusion |
65% |
73.5% |
p<0.05 |
| PT following transfusion |
75% |
78.5% |
|
| aPTT prior to transfusion |
46 s |
38.5 s |
p<0.05 |
| aPTT following transfusion |
50 s |
40 s |
|
| Platelets |
|
|
|
| Number of platelets... |
with indication |
without indication |
|
| prior to transfusion |
42.5 G/L |
179 G/L |
p<0.05 |
| following transfusion |
71.5 G/L |
166 G/L |
|
| |
With suspected thrombocytopathy |
Without suspected thrombocytopathy |
|
| prior to transfusion |
100 G/L |
49 G/L |
p=0.0404 |
*Risk factors such as acute respiratory distress syndrome (ARDS), shock, sepsis, multiple trauma, massive blood loss postoperatively/gastrointestinal (GI) bleedings
Table 5: Transfusion triggers for transfused patients.
Guideline divergent plasma transfusion is not capable to change lab values for PT and aPTT (p<0.05).
The effect of platelet transfusion upon pre-transfusion platelet counts is associated to guideline conformity, indicating that a significant change could not be achieved by a not guidelineconform indication. The transfusion trigger “thrombocytopathy” increases the platelet threshold to 100 g/L.
Discussion
This is the first report about transfusion practice in critically ill patients in Germany. Although especially the German guideline recommendations are very detailed and are supported by variable strength of recommendation derived from evidence and grading, in approximately a third of investigated blood products guideline coverage could not be found. This result confirms aroused suspicions from the German IAKH error registry of blood products that the clinical use of blood has a high percentage of errors. The study might indicate a misuse of blood products doing ethical harm, as well as avoidable health care cost charging the health care society but also a potential harm to patients by unnecessary exposure to allogeneic blood. On the other hand, the study also demonstrates that complexity of the critical illness is a major explanation for liberal transfusion management and overtransfusion with all blood components.
The comparable degree of guideline discordance for all blood products indicates that the German system of transfusion practice still is not convinced by underlying evidence: For red cells, intensive care physicians still are using hemoglobin concentrations higher than 8 g/L as transfusion trigger, in a third of applications in stable patients without documented clinical symptoms. This is approximately consistent with "historical" studies but in contrast to existing guidelines. A clear reason remains speculative. For the double unit transfusion, a more procedural explanation arises - in more than half of cases (57.43%) a double as opposed to a single unit of PRC was demanded and administered. Consequently over transfusion could be demonstrated in this study by exceeding post transfusion Hb content. For this, multiple obstacles to the recommended single unit procedure seem to be responsible - it doubles work, delays the time to reach the target hemoglobin level and requires more attention by adding the additional step after the first unit. If the ordering physician is not aware of the risk of each unit of blood, the process is shortcut and simplified by a double unit order and administration. If this common practice can be avoided, the overall transfusion rate decreases and acquisition cost for blood is reduced [12]. A successful method to promote single-unit orders was achieved by special software for blood orders by either requesting a guideline covered indication (uncontrolled bleeding, instability) or restrict the order mode to single units. Within three subsequent observation years, it was able to decrease transfused units per day and double-unit transfusion by more than two-fold. [12].
In almost two thirds of applications (69.5%, average dose 7.27 ml/kg), plasma was transfused in insufficient doses [18]. One possible reason was the low sensitivity of routine laboratory parameters to indicate a coagulation disorder and the waiting period for the result. Harmful or ineffective plasma overuse [13- 15] and prophylactic use [16-18] in critical ill patients could be overcome by coagulation concentrates [19].
Similarly, a third of platelet administrations were not in congruence with guideline recommendations due to assumed dysfunction. Platelet function measurement is not established ubiquously and therefore guidelines refer to number counts. Almost 70% of platelet administrations in this ICU were motivated by dysfunction, being performed at platelet counts above 100 g/L. It seems that transfusion triggers given in guidelines are not specific enough for critically ill patients. For both plasma and platelets, establishment of point of care testing such as impedance aggregometry or PFA analysis might reduce transfusion rate, save cost and probably improves outcome [20]. In a multicenter study, the implementation of point of care testing reduced massive transfusion events by half, reduced plasma, red cell and platelet transfusion to respective maximal effects of reducing transfusion in 90% for FFP, 62% in RBC and 72% in platelets [21].
Considering the quality and accuracy of the transfusion guidelines of the German Medical Association, thirty percent of non-compliance seems to be quiet high. The search for an easy explanation requires the inclusion of various contributing factors. Napolitano and coworkers discuss the strength of underlying evidence and the level of acceptance of the recommending institution as critical factors for the speed and intensity for guideline implementation [22]. Thus, low evidence levels or doubts addressing the methodology underlying the restrictive transfusion recommendation are a reason for malcompliance among physicians as recently addressed [23-25]. However, especially recommendations with high evidence such as the prophylactic use of plasma were not adhered to in this study or other settings by a higher degree. In cirrhosis, prophylactic transfusion in the absence of planned procedure is widely (61%) used although not covered by evidence [26]. Furthermore, the complexity of clinical situations for critically ill patients might be contributing. In a Dutch study of general practitioners treating multimorbidity, the integration of patient-specific factors in medical decisions and the aim for patient-centered solutions was found to be interfering with applicability of guidelines [27]. However, in anticipation of the complexity of critical illness and its impact on transfusion behavior in this study, we already included transfusion categories for every blood product that were not exactly addressed in the guidelines. Although it might not compensate for the whole extent of malperformance, the results of this retrospective analysis do not support a major impact of critical illness upon the lack of guideline adherence.
Limitations of this study contributing to obtained results need further consideration. Many indications of blood products might be missed since this study was retrospective. However, the chart review was performed thoroughly and in close cooperation with the same ICU physicians in charge. Also, documentation of transfusion needs and success in the chart is common practice and part of guideline adherence. If no documentation was found, any other given reason for transfusion in accordance to guidelines was checked by blood losses and laboratory values. However, if documentation of blood loss equals clinical symptoms of ischemia in stringency and accuracy is debatable. Although troponin levels and EKG tracings, neurology consultations were reviewed, some suspicions of ischemia triggered the decision to transfuse (according to the interviews with the ICU physicians). Therefore, ischemia triggered RBC transfusion might have remained undocumented in some cases. German physicians are held to prove and document anemia symptoms, as well they are instructed to quit the habit of prophylactic blood use. In this study, especially for FFP and PC, the documentation of transfusion indication was missing in a considerable part of administrations. The explanation by ICU physicians that many clinical situations are not covered by guidelines seems too deliberate. Especially for platelets, an extensive number of clinical scenarios are covered by German guidelines.
Another issue should be considered: If we selected an institution with a low compliance to guideline adherence and transfusion medicine, the results would not be representative for German institutions. In the opposite, we selected a high quality and renowned teaching university level one trauma center and ICU with a very active and clinicaly involved transfusion medicine department. In consequence, the results obtained in this study can be considered representative, although performance and guideline adherence might be higher in a few other institutions in Germany, and even lower in many others.
However, what measure will improve guideline adherence? Actual medical information and Continuous Medical Education (CME) is best organized in university hospitals with large teaching facilities such as in our center. The impact of CME is poorly defined in relation to clinical outcomes, and efforts to standardize definitions of clinical outcomes are in varied stages of development [28]. Thus, there is no clear evidence that mandatory information and education as well as didactic education and passive dissemination strategies are effective in successful guideline implementation strategies [29]. According to authors of a recent assessment, effective implementation strategies included multifaceted interventions, interactive education and clinical reminder systems. The latter in the field of transfusion of blood and blood products might be software based solutions such as a monitoring and feedback program [30] or software enforcing guideline adherence [31-33]. Also, an intensive workshop for a week, a “transfusion camp”, was very successful for transfer of transfusion knowledge to clinicians [34]. In conclusion, practice based educational together with profound electronic support might be the necessary method to improve guideline adherence in Germany.
Conclusion
In conclusion, transfusion guidelines were not followed by critical care physicians of a German university center in more than a third of applications. Double red cell unit administrations, under dosed plasma transfusion and platelet overuse together with a liberal attitude towards blood transfusion for critical ill were evaluated in this retrospective study. One reason for poor compliance might be the complexity of critical illness. Intensive education together with electronic support might be the most promising methods to improve compliance to guidelines.
References
- Gombotz H, Rehak PH, Shander A, Hofmann A (2007) Blood use in elective surgery: The Austrian benchmark study. Transfusion 47: 1468-1480.
- Gombotz H, Rehak PH, Shander A, Hofmann A (2014) The second Austrian benchmark study for blood use in elective surgery: Results and practice change. Transfusion 54: 2646-2657.
- Meier J, Filipescu D, Kozek-Langenecker S, Llau Pitarch J, Mallett S, et al. (2016) Intraoperative transfusion practices in Europe. Br J Anaesth 116: 255-261.
- Lucas DJ, Ejaz A, Spolverato G, Kim Y, Gani F, et al. (2016) Packed red blood cell transfusion after surgery: Are we "over tranfusing" our patients? Am J Surg 212: 1-9.
- Fillet AM, Desmarets M, Assari S, Quaranta JF, Francois A, et al. (2016) Blood products use in France: A nationwide cross-sectional survey. Transfusion 56: 3033-3041.
- Hoppe JD, Cichutek K, SkrIba PC (2010) Richtlinien zur Gewinnung von Blut und Blutbestandteilen und zur Anwendung von Blutprodukten (Hämotherapie). In: Paul-Ehrlich-Institut BriEmd, editor. 2. Anpassung 2010 ed: Bundesanzeiger
- Bundesärztekammer (2009) Cross-sectional guidelines for therapy with blood components and plasma derivatives. Transfus Med Hemother 43: 223-232.
- Gesetz zur Regelung des Transfusionswesens (Transfusionsgesetz - TFG) (1998).
- Frietsch T, Weiler-Lorentz A, Schipplick M, Kretschmer V (2009) The German interdisciplinary taskforce for clinical hemotherapy IAKH and its national critical incident reporting system specifically for blood transfusion. Anasthesiol Intensivmed Notfallmed Schmerzther 44: 626-628.
- Hebert PC (1999) Anemia and red cell transfusion in critical care. Transfusion requirements in critical care investigators and the Canadian Critical Care Trials Group. Minerva Anestesiol 65: 293-304.
- DKG DK (2015) Kosten der Blutprodukte DKG
- McKinney ZJ, Peters JM, Gorlin JB, Perry EH (2015) Improving red blood cell orders, utilization and management with point-of-care clinical decision support. Transfusion 55: 2086-2094.
- Chowdary P, Saayman AG, Paulus U, Findlay GP, Collins PW (2004) Efficacy of standard dose and 30 ml/kg fresh frozen plasma in correcting laboratory parameters of haemostasis in critically ill patients. Br J Haematol 125: 69-73.
- de Almeida JP, Palomba H, Galas FR, Fukushima JT, Duarte FA, et al. (2012) Positive fluid balance is associated with reduced survival in critically ill patients with cancer. Acta Anaesthesiologica Scandinavica 56: 712-717.
- de Almeida JP, Vincent JL, Galas FR, de Almeida EP, Fukushima JT, et al. (2015) Transfusion requirements in surgical oncology patients: A prospective, randomized controlled trial. Anesthesiology 122: 29-38.
- Banerjee D, Hussain R, Mazer J, Carino G (2014) A prophylactic fresh frozen plasma transfusion leads to a possible case of transfusion-related acute lung injury. BMJ Case Rep.
- Gorlinger K, Saner FH (2015) Prophylactic plasma and platelet transfusion in the critically Ill patient: Just useless and expensive or even harmful? BMC Anesthesiol 15: 86.
- Pieters BJ, Conley L, Weiford J, Hamilton M, Wicklund B, et al. (2015) Prophylactic versus reactive transfusion of thawed plasma in patients undergoing surgical repair of craniosynostosis: A randomized clinical trial. Paediatr Anaesth 25: 279-287.
- Muller MC, Straat M, Meijers JC, Klinkspoor JH, de Jonge E, et al. (2015) Fresh frozen plasma transfusion fails to influence the hemostatic balance in critically ill patients with a coagulopathy. J Thromb Haemost 13: 989-97.
- Whiting P, Al M, Westwood M, Ramos IC, Ryder S, et al. (2015) Viscoelastic point-of-care testing to assist with the diagnosis, management and monitoring of haemostasis: A systematic review and cost-effectiveness analysis. Health Technol Assess (Winchester, England) 19: 1-228.
- Gorlinger K, Fries D, Dirkmann D, Weber CF, Hanke AA, et al. (2012) Reduction of fresh frozen plasma requirements by perioperative point-of-care coagulation management with early calculated goal-directed therapy. Transfus Med Hemother 39: 104-113.
- Napolitano LM, Kurek S, Luchette FA, Corwin HL, Barie PS, et al. (2009) Clinical practice guideline: Red blood cell transfusion in adult trauma and critical care. Crit Care Med 37: 3124-3157.
- Klein HG, Cortes-Puch I, Natanson C (2015) Clinical practice: Blood-transfusion decisions not simple. Nature 521: 289.
- Klein HG, Flegel WA, Natanson C (2015) Red blood cell transfusion: Precision vs. imprecision medicine. JAMA 314: 1557-1558.
- Van Remoortel H, De Buck E, Dieltjens T, Pauwels NS, Compernolle V, et al. (2015) Methodologic quality assessment of red blood cell transfusion guidelines and the evidence base of more restrictive transfusion thresholds. Transfusion.
- Desborough MJ, Hockley B, Sekhar M, Burroughs AK, Stanworth SJ, et al. (2015) Patterns of blood component use in cirrhosis: A nationwide study. Liver Int.
- Luijks H, Lucassen P, van Weel C, Loeffen M, Lagro-Janssen A, et al. How GPs value guidelines applied to patients with multimorbidity: A qualitative study. BMJ Open 5: 007905.
- Mazmanian PE, Davis Da Fau - Galbraith R, Galbraith R (2009) Continuing medical education effect on clinical outcomes: Effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest 135: 49-55
- Prior M, Guerin M, Grimmer-Somers K (2008) The effectiveness of clinical guideline implementation strategies--a synthesis of systematic review findings. J Eval Clin Pract 14: 888-1897.
- Mehra T, Seifert B, Bravo-Reiter S, Wanner G, Dutkowski P, et al. (2015) Implementation of a patient blood management monitoring and feedback program significantly reduces transfusions and costs. Transfusion 55: 2807-2815.
- Chang CS, Lin YC, Lin CC, Yeh CJ, Wu YC, et al. (2012) The physician compliance of red blood cell transfusion by computerized transfusion decision support system. Kaohsiung J Med Sci 28: 331-335.
- Goodnough LT, Shah N (2014) The next chapter in patient blood management: Real-time clinical decision support. Am J Clin Pathol 142: 741-777.
- Rothschild JM, McGurk S, Honour M, Lu L, McClendon AA, et al. (2007) Assessment of education and computerized decision support interventions for improving transfusion practice. Transfusion 47: 228-239.
- Lin Y, Cserti-Gazdewich C, Callum J (2015) Evaluation of "Transfusion Camp," a postgraduate transfusion medicine education program using the BEST-TEST knowledge assessment tool. Transfusion 55: 2049-2051.