Aysel Özenergün-BittacÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñ1, Havva Ozge Keseroglu1*, Müzeyyen Gönül1, Ahmet TuÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâ¦Ã¸rul Su1, AyÃÆÃââââ¬Ã¦ÃÆââ¬Å¡Ãâ¦Ã¸egül AdabaÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâ¦Ã¸2 and Dilek Koyuncu2
1Department of Dermatology, DÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñÃÆÃââââ¬Ã¦ÃÆââ¬Å¡Ãâ¦Ã¸kapÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñ YÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñldÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñrÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñm BeyazÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñt Education and Research Hospital, Ankara, Turkey
2Department of Pathology, DÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñÃÆÃââââ¬Ã¦ÃÆââ¬Å¡Ãâ¦Ã¸kapÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñ YÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñldÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñrÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñm BeyazÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñt Education and Research Hospital, Ankara, Turkey
- *Corresponding Author:
- Havva Ozge Keseroglu
Department of Dermatology, DÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñÃÆÃââââ¬Ã¦ÃÆââ¬Å¡Ãâ¦Ã¸kapÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñ YÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñldÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡ÃâñrÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñm BeyazÃÆÃââââ¬Ã
¾ÃÆââ¬Å¡Ãâñt Education and Research Hospital, 06110, Ankara, Turkey.
Tel: +903125962000
E-mail: ozgederm@yahoo.com
Received Date:October 27, 2015; Accepted Date: November 12, 2015; Published Date: November 20, 2015
Citation: Özenergün-Bittaci A, Keseroglu HO, Gönül M, et al. A Case of Eczema Herpeticum Occurring on the Lesions of Pemphigus Foliaceus. Clin Pediatr Dermatol. 2016, 1:1. doi: 10.21767/2472-0143.100005
Eczema herpeticum is the cutaneous dissemination of a viral infection in the setting of an underlying chronic skin condition. We would like to report a rare case of 18- year old man with a pemphigus foliaceus who developed disseminated cutaneous herpes simplex infection. In this report, we want to emphasize the difficulties in the diagnosis of eczema herpeticum when it occurs on the background of pemphigus.
Keywords
Eczema herpeticum; Pemphigus foliaceus; Herpes simplex virus
Introduction
Eczema herpeticum [EH] is the cutaneous dissemination of a viral infection in the setting of an underlying chronic skin condition [1-3]. Occurrence of EH on the pemphigus foliaceus [PF] lesions is very rare [4,5].
Case
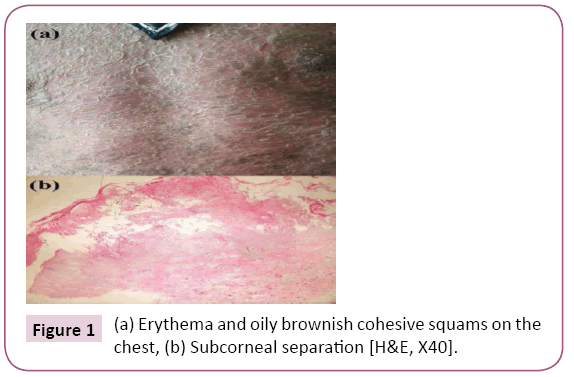
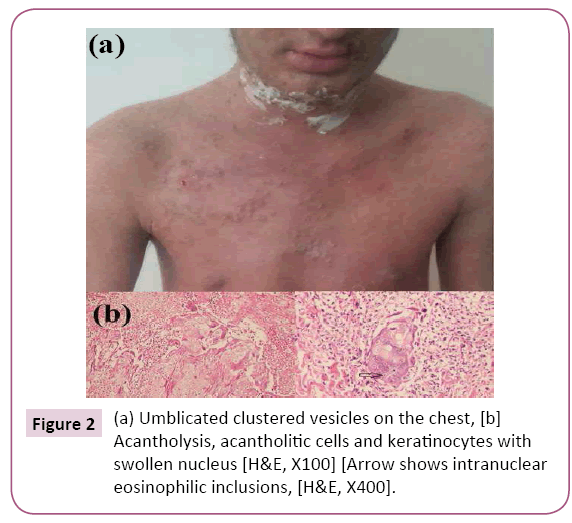
An 18-year old man was attended with generalized erythema and desquamation gradually spreading for 1 month. Dermatological examination showed erythema and oily brownish cohesive squams on whole body (Figure 1a). Subcorneal separation in the histopathological examination (Figure 1b) and positive pericellular staining with immunoglobulin G supported the diagnoses of PF. The lesions were still resistant to oral prednisolon [90 mg/d] and azathioprine [150 mg/d] treatments after one month [only desquamation regressed]. The patient got fever [38°C] and new crusted and grouped, painful umblicated vesicles appeared on the lips, neck, right axillae, chest and groin (Figure 2a). Intranuclear eosinophilic inclusions were detected on the histopathological examination of these lesions and he was diagnosed as EH occurred on the PF lesions (Figure 2b). Anti-herpes simplex virus [HSV]-1 IgM and IgG antibodies were positive. These lesions disappeared and body temperature became normal range with intravenous acyclovir therapy [5 mg/kg × 3/day]. Intravenous immunoglobulin therapy was added to the treatment because of persisting erythroderma. PF lesions almost completely regressed within two weeks.
Figure 1: (a) Erythema and oily brownish cohesive squams on the chest, (b) Subcorneal separation [H&E, X40].
Figure 2: (a) Umblicated clustered vesicles on the chest, [b] Acantholysis, acantholitic cells and keratinocytes with swollen nucleus [H&E, X100] [Arrow shows intranuclear eosinophilic inclusions, [H&E, X400].
Discussion
EH is a rarely seen infection of the HSV. EH begins as a sudden eruption of painful, edematous, often crusted or hemorrhagic vesicles, pustules or erosions in areas of the preexisting dermatosis. EH has been reported in acyclovir therapy, pityriasis rubra pilaris, psoriasis, seborrheic dermatitis, Darier's disease, Hailey-Hailey disease, bullous pemphigoid and ichthyosis vulgaris [1,3]. The occurrence of eczema herpeticum over the PF is very rare, so that only 14 cases have previously been reported in the literature [2,4,5]. The pathogenesis of EH is unknown however it has been thought that impaired barrier function of the epidermis may cause the development and spreading of infection [3,5]. Patients with immunodeficiency are more susceptible to herpetic infection because of alteration of humoral and/or cellular immunity [5]. It may be the primary factor in dissemination of the viral infection as seen in our case. All of the cases previously reported were using steroids with or without other immunosuppressive treatment at the time of diagnosis, as in our case. It was proposed that the severity of the herpetic infections was related to immunosuppressed state rather than the steroid dosage [2,4]. The diagnosis of EH may be difficult when it occurs in the setting of pemphigus. Tzanck test, viral culture, serology, histopathological examination and DIF may confirm the diagnosis of EH but we think that the most important step in diagnosis is to remember the possibility of EH [3]. HSV types 1 or 2 were detected in the lesions of patients previously reported [4]. In our patient, anti HSV-1 IgM and IgG antibodies were positive and histopathological examination revealed intranuclear eosinophilic inclusions suggesting the possibility of viral infection.
Antiviral therapy should not be delayed because EH can be life threatening. There has been one fatal case among these 15 patients with PF superinfected with HSV [4]. The treatment with high-dose IV acyclovir is the most commonly used therapy [3]. Our case responded quickly to high-dose IV acyclovir therapy. We presented a very rare case of EH in the setting of PF. The diagnosis of EH is quite important when it occurs in the setting of bullous dermatoses because vesiculobullous lesions were present in both disease. If EH is misinterpreted as deterioration of the underlying bullous disorder in a patient with bullous dermatosis unresponsive to immunosuppressive therapy, as in our patient, this may result in inappropriate treatment with enhanced immunosuppression and even death. So, it is important that EH should be kept in mind as differential diagnosis in newly existing bullous lesions in a patient with PF.
References
- Leung DYM, Eichenfied LF, Boguniewicz M (2012) Atopic dermatitis (Atopic eczema). In: Fitzpatrick’s Dermatology in General Medicine [Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, eds.] 8th edn. McGraw-Hill:New York 165-182.
- Palleschi GM, Falcos D, Giacomelli A, Caproni M (1996) Kaposi's varicelliform eruption in pemphigus foliaceus. Int J Dermatol 35:809-810.
- Olson J, Robles DT, Kirby P, Colven R (2008) Kaposi varicelliform eruption (eczema herpeticum). Dermatol Online J14:18.
- Demitsu T, Kakurai M, Azuma R, Hiratsuka Y, Yamada T, et al. (2008) Recalcitrant pemphigus foliaceus with Kaposi's varicelliform eruption: report of a fatal case. Clin Exp Dermatol 33:681-682.
- Rao G, Chalam KV, Prasad GP, Sarnathan M, Kumar H (2007) Mini outbreak of Kaposi's varicelliform eruption in skin ward: a study of five cases. Indian J Dermatol Venereol Leprol 73:33-35.